Director, Medical Student Education
Assistant Professor of Anesthesiology
Anesthesiology is a large specialty and encompasses operating room anesthesia services, perioperative medicine, critical care, and pain medicine. Duke Anesthesiology provides care for more than 40,000 patients each year across a wide range of disciplines, providing students with extensive experience and challenging them to consider the management of patients in the perioperative period. For the second consecutive year, US News & World Report (USNWR) ranked Duke University's Department of Anesthesiology #3 in the nation for "Best Medical Schools for Anesthesiology," sustaining our highest ranking since USNWR began including anesthesiology in its specialty rankings in 2018.
Students can experience a range of general as well as regional anesthesia cases, discuss the preparation and planning for cases, better understand the perioperative pain management options, review the perioperative medications, calculate the correct dosing and choice of intravenous fluids (including blood transfusion therapy) and also plan postoperative care. Additionally, our students have the opportunity to learn airway management skills in the Duke Human Simulation and Patient Safety Center, which they can apply in the operating room. They can also participate in vascular access techniques and a spectrum of point-of-care ultrasound skills during the care of patients.
For students, a mixture of practical skills, basic science knowledge, and clinical problem-solving unfold in a fast-paced environment that touches on many topics covered in preclinical classes.
Anesthesiologists interact with students in all four years of the medical student curriculum, providing education in a wide variety of formats, including traditional didactics, problem-based learning, small groups, tutorials, and utilizing the simulation center.
For visiting medical students interested in rotations, please visit the Duke University School of Medicine Visiting Medical Student website, where all visiting student requirements are explained. After reviewing the School of Medicine Visiting Medical Students website, questions can be directed to Scott Campbell, scott.campbell@duke.edu, for more information about the application process. Acceptance to a visiting student rotation in the Department of Anesthesiology is based on availability. We encourage you to apply broadly to our courses in order to increase your chances of acceptance. Acceptance for a visiting student rotation does not guarantee a residency interview.
To learn more about our courses, please click through the information below for course curricula and objectives. Actual course content can vary depending on the time of year and current education initiatives.
Courses
ANESTH-205C Anesthesia Clerkship Rotation. All Duke medical students will spend one week learning the basics of anesthesia and perioperative medicine. Class didactics paired with online learning, plus simulation center teaching on airway skills and intravenous cannulation, are supplemented with exposure to operating room anesthesia. Knowledge and skills that are applicable to all interns will be emphasized, including the pharmacology and physiology behind safe care of the patient in the operating room, fluid resuscitation, acid-base status, blood transfusion, crisis resource management, and patient safety. Pain management will also be addressed including safe opioid prescribing practices. The course director is Dr. Grace McCarthy.
ANESTH-220C Clinical Anesthesia. The one-week selective permits students with an interest in perioperative medicine to rotate through multiple anesthesia subspecialties. The clinical opportunity is supplemented by teaching in the simulation center and didactic opportunities in the department. The course director is Dr. Sophia Dunworth
ANESTH-221C Chronic Pain. In addition to the selective in anesthesiology, there is a selective in pain management. This selective provides exposure to outpatient interventional pain management. Students will see patients in the Duke Pain Medicine clinic, fluoroscopy suite, and procedural operating room. The course director is Dr. Lance Roy.
ASEP Program. While the university offers a range of opportunities from biochemistry to organ physiology, anesthesiology, surgery, and critical care integrate these multiple systems into a larger perspective of human pathophysiology and pharmacology. Students have opportunities for research in cardiovascular and respiratory physiology, molecular pharmacology, neurobiology, and environmental science. Regardless of ultimate career choice, investigation in anesthesiology, surgery, critical care medicine, and environmental physiology provides a strong basic science grounding and application of research principles. To explore opportunities for research in our department, click on the Research Guide below. There are also opportunities for third year continuity clinics. Please contact Dr. Grace McCarthy if interested.
ANESTH-440C Anesthesia. Fourth-year students can participate in the perioperative anesthetic management of patients while assigned to an individual resident or attending anesthesiologist. The close interaction with faculty and residents is based around rotations of approximately two weeks in the general operating rooms - one in the cardiothoracic operating rooms, and a fourth week in subspecialty areas, including Duke’s hyperbaric facility, the Acute Pain Management Service, and others. Learning opportunities will include preoperative patient evaluation, anesthetic technique selection, airway management, pharmacology, physiology, and anatomy, as well as procedures such as ultrasound-guided vascular access, including central venous and arterial line placement, and patient monitoring. These areas will be reinforced by lectures, Grand Rounds, and an innovative problem-based learning series that builds through the rotation. The course director is Dr. Abigail Melnick.
ANESTH-401C Cardiothoracic Critical Care Elective and ANESTH-402C Cardiothoracic Critical Sub-I. The cardiothoracic intensive care sub-internship or elective will allow fourth-year medical students to be exposed to and participate in the care of the postoperative and critically ill cardiac and thoracic surgery patients. This patient population has the highest rate of invasive monitoring, echocardiographic and hemodynamic assessment, and advanced circulatory support, including utilization of inotropes, vasopressors, and mechanical circulatory support devices (LVAD, RVAD, IABP). A working knowledge of these concepts will be critical to a future career in anesthesiology, critical care medicine, or surgery.
Critical care medicine has evolved from a discipline where one or two organ systems are supported during critical illness to one where technological advances allow us to support virtually all organ systems. The CTICU (7W) utilizes the highest variety of circulatory support and a wide variety of support of other organ systems. Physicians practicing in the 21st century will need a working knowledge of these devices, the opportunities they offer, and their shortcomings. The course director is Dr. Michael Cutrone.
ANESTH-441C. Critical Care Sub-I. Students engaging in the Surgical Intensive Care Unit (SICU) sub-internship will gain hands-on experience and broad-based knowledge in managing critically ill surgical and trauma patients. Students will take ownership of a panel of patients under the supervision of Anesthesia and Trauma/Surgical Critical Care attendings and housestaff and actively participate in daily rounds as part of the SICU team. Didactics will include multiple weekly scheduled and informal lectures. Students take one week of four-night call and work one-on-one with SICU house staff in the supervised management of critically ill patients. Time may be spent in the SICU at Duke University Medical Center (trauma, vascular surgery, liver-kidney-pancreas transplantation, general surgery) and/or the SICU at the Durham VA Medical Center (cardiothoracic and vascular surgery, general surgery). Instruction on the rotation will include particular emphasis on procedures and techniques necessary for Critical Care, including hemodynamic assessment and monitoring, cardiovascular resuscitation and use of vasoactive drugs, ventilator management such as ARDS, prevention, and management of nosocomial infections, and ethical decision-making in the ICU. The SICU house staff and the attending physician formally evaluate students. The course directors are Dr. Adjoa Boateng-Evans and Dr. Taylor Herbert.
ANESTH-446C Acute and Chronic Pain Management. This course is offered to fourth-year medical students within Duke Anesthesiology. During this four-week elective, students will participate in both inpatient and outpatient pain management. Each student is assigned daily to an individual fellow or attending physician who supervises the student’s active involvement. This involvement emphasizes a multidisciplinary approach appropriate for the individual patient. Topics reviewed include opioid and non-opioid management, interventional procedures such as epidural and peripheral nerve catheter placement, nerve blocks, neurolytic procedures, as well as implantable devices. The benefits of physical and psychological therapy are stressed. Students will observe and/or participate in various interventional procedures. In addition to this clinical work, students attend a pain conference and weekly grand rounds. The course is offered during each elective period throughout the year. The course director is Dr. Lance Roy.
ANESTH-430C. Diving and Hyperbaric Medicine. Students participate actively in assigned patient care and clinical projects to educate learners through the discussion of altered environmental conditions as related to human physiology and ultimately patient care. Students will work directly on a team with attending physicians, fellows, residents, and hyperbaric staff. Diving and Hyperbaric/Hypobaric medicine consultative services are provided by the team for fitness-to-dive evaluations, emergency patients, inpatients, and outpatients referred by a variety of services including emergency medicine, intensive care units, orthopedics, vascular surgery, otolaryngology, medicine, radiation oncology, and preoperative/postoperative care units. Specific indications for hyperbaric oxygen therapy are discussed throughout the course and students are mentored in the assessment of divers and patients referred for hyperbaric therapy. As knowledge of the field increases, students are encouraged to take on progressive responsibility in learning to manage the clinical service with guidance in a respectful learning environment. Students will have opportunities to directly evaluate patients, give patient presentations, communicate with outside services, follow up on patient care-related tasks, and lead weekly rounds. Feedback is provided on a real-time basis. Students are also expected to give an “end-of-rotation” academic presentation. For more information, please contact Bruce Derrick, MD or Esther Turner. Students should meet for rounds on the first day of classes promptly at 7:30 am. The location is Hyperbaric Center Library, 0588 White Zone, CR II Building. Credit: 4. Enrollment Max 2 per block. The course director is Bruce Derrick, MD, and staff.
ANESTH-445C. Physiology & Medicine of Extreme Environments. Advanced topics in the physiology and medicine of altered ambient pressure, immersion, gravity, temperature, and breathing gas composition. Environments considered include diving and hyperbaric medicine; exercise physiology; hot/cold terrestrial and water operations; microgravity and high-g acceleration; high altitude; and space medicine. Basic mechanisms and medical management of associated diseases are examined including decompression sickness, altitude sickness, hypothermia and hyperthermia, hypoxia, carbon dioxide and carbon monoxide poisoning, and oxygen toxicity. Practical applications: pressure vessel design and operation, life support equipment, cardiorespiratory physiology measurements at low and high pressure, optional simulated chamber dive and/or flight. Attendance, either online via Zoom or in person is mandatory unless otherwise approved by the course director in advance. The course meets weekly on Thursday evenings from 5:00 pm until 7:30 pm beginning in January for 8 weeks. For more information, contact Bruce Derrick, MD or Esther Turner. Credit: 1, Non-Direct Patient Care credit. Enrollment: max 20, min. 10. The course directors are Bruce Derrick, MD, and Richard Moon, MD
Anesthesiology Interest Group
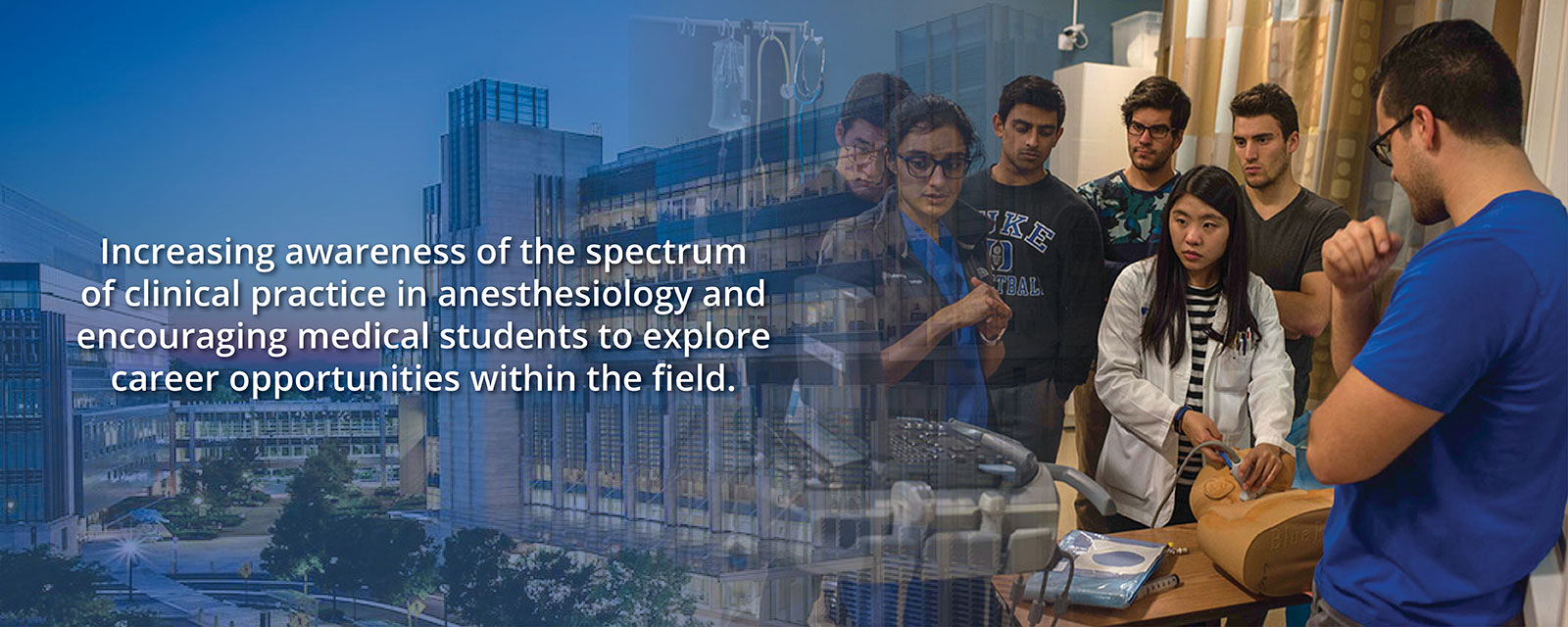
To raise awareness about the diverse clinical practices in anesthesiology and inspire medical students to consider careers in this field.
The Anesthesiology Interest Group (AIG) at Duke University School of Medicine aims to provide broader exposure to anesthesiology beyond the standard curriculum. This includes mentorship, educational opportunities, and hands-on experiences with Duke Anesthesiology faculty and residents.
Goals of the Anesthesiology Interest Group (AIG):
- Education:
- Offer lectures, discussions, research presentations, and informal social events to educate medical students about anesthesiology.
- Skill Development:
- Provide hands-on workshops and physician shadowing programs to help students learn the technical skills essential to anesthesiology.
- Mentorship:
- Pair interested medical students with faculty members and residents for mentorship opportunities.
- Achievements:
- Recognized as the 2024 Outstanding Anesthesiology Interest Group in the Best Overall AIG category by the ASA Medical Student Component.
We encourage Duke University students to accompany an anesthesiologist to the Operating Room or other clinical or research settings such as the Intensive Care Units, the Hyperbaric Center, or the Duke Pain Medicine clinic. If you are interested, please contact Dr. Grace McCarthy or Dr. Abigail Melnick, the AIG co-chairs, for recommendations and introductions. Below is a listing of current Duke Anesthesiology faculty to provide you with an idea of the wide variety of options available.
Ambulatory
Alex Cravanas, MD
Mike Kent, MD
Cardiothoracic
Brandi Bottiger, MD
Nazish Hashmi, MD
Negmeldeen Mamoun, MD, PhD
Sharon McCartney, MD
Angela Pollak, MD
Mark Stafford-Smith, MD
Annemarie Thompson, MD
Meredith Whitacre, MD
Critical Care Medicine
Sandy An, MD
Kathleen Claus, MD
Mike Devinney, MD
Amanda Faulkner, MD
Taylor Herbert, MD
Ehis Iboaya, MD
Nancy W. Knudsen, MD
Vijay Krishnamoorthy, MD
John T. Lemm, MD
Rachel Mintz-Cole, MD
Karthik Raghunathan, MBBS, MPH
Galen Royce-Nagel, MD
Arturo Suarez, MD
Christopher C. Young, MD
General, Vascular, High-Risk Transplant (GVT)
Chakib Ayoub, MD
Jeanna Blitz, MD
Brian Colin, MD
Sarada Eleswarpu, MD
Arun Ganesh, MD
Richard E. Moon, MD
Ankeet Udani, MD
Kerri M. Wahl, MD
David Williams, MD
Christopher C. Young, MD
Hyperbaric Medicine
Richard E. Moon, MD
Neuroanesthesiology
Miles Berger, MD
Andrew Peery, MD
Bret W. Stolp, MD
Pain Management
Scott Runyon, MD
Kevin Vorenkemp, MD, FASA
Peter Yi, MD
Pediatric
Wads Ames, MD
John B. Eck, MD
Lisa Einhorn, MD
Eddie Jooste, MD
Elizabeth Malinzak, MD
Annie Udani, MD
Regional
Mike Bullock, MD
Josh Dooley, MD
Jeffrey Gadsden, MD
Amanda Kumar, MD
David MacLeod, MD
Brian Ohlendorf, MD
Neil Ray, MD
VAMC
John Hsia, MD
Eric Johnbull, MD
David Lindsay, MD
Grace McCarthy, MD
Srini Pyati, MD
Lance Roy, MD
Rebecca A. Schroeder, MD
Tom Van de Ven, MD, PhD
Women's
Melissa Bauer, DO
Jennifer Dominguez, MD
Abigail H. Melnick, MD
Marie-Louise Meng, MD
Adeyemi J. Olufolabi, MB
Cam Taylor, MD
Mary Yurashevich, MD

2nd Year One-Week Electives
ANES 220C: Clinical Anesthesiology
Students will participate in the pre-, intra-, and post-operative anesthetic management of patients while assigned 1:1 to an anesthesiologist. For more information, please contact Dr. Grace McCarthy or Esther Turner, 919-681-6437. See Course Catalog at dukehub.duke.edu for full course description.
ANES 221C: Pain Management
Students participate in both outpatient and inpatient chronic pain management. This course emphasizes a multidisciplinary approach, with emphasis on pharmacotherapy, interventional procedures, physical therapy, and psychological therapy. Students with questions may contact: Dr. Lance Roy or Esther Turner, 919-681-6437. See Course Catalog at dukehub.duke.edu for full course description.
4th Year Four-Week Electives
ANESTH 401C: CTICU Sub-Internship
Allows fourth year medical students to be exposed to and participate in the care of the post-operative and critically ill cardiac and thoracic surgery patient. Satisfies the sub-internship requirement for graduation. For more information, contact Dr. Sharon McCartney or Esther Turner, 919-681-6437. See Course Catalog at dukehub.duke.edu for full course description.
ANESTH 402C: CTICU Elective
Allows fourth year medical students to be exposed to and participate in the care of the post-operative and critically ill cardiac and thoracic surgery patient. Satisfies the acute care requirement for graduation. For more information, contact Dr. Sharon McCartney or Esther Turner, 919-681-6437. See Course Catalog at dukehub.duke.edu for full course description.
ANESTH 430C: Diving and Hyperbaric Medicine
Students participate actively in assigned patient care and clinical projects. Specific indications for hyperbaric oxygen therapy are used in clinical care and in developing translational projects. For more information, please contact Dr. Bruce Derrick, 919-668-0032. See Course Catalog at dukehub.duke.edu for full course description.
ANESTH 440C: Clinical Anesthesiology
Students participate in the pre-, intra-, and post-operative anesthetic management of patients in the general operating rooms, the cardiothoracic operating rooms, and in various subspecialty areas, such labor and delivery, pediatric operating rooms, neurosurgical operating rooms, regional anesthesiology service, and/or acute pain management. Satisfies the acute care requirement for graduation. For questions and to obtain permission numbers, please contact Esther Turner, 919-681-6437. See Course Catalog at dukehub.duke.edu for full course description.
ANESTH 441C: SICU Sub-Internship
Under supervision, students function as sub-interns in the Surgical Intensive Care Unit (SICU) in 6 West DMP. Students are assigned their own patients and actively participate in daily rounds as part of the SICU team. Satisfies the sub-internship requirement for graduation. See Course Catalog at dukehub.duke.edu for full course description.
ANESTH 445C: Physiology & Medicine of Extreme Environments
Advanced topics in the physiology and medicine are altered ambient pressure, immersion, gravity, temperature, breathing gas composition and hibernation. Environments considered include: diving and hyperbaric medicine; hot/cold terrestrial and water operations; microgravity and high-g acceleration; high altitude; space. For more information, contact Dr. Bruce Derrick. See Course Catalog at dukehub.duke.edu for full course description.
ANESTH 446C: Acute and Chronic Pain Management
Students learn a multidisciplinary approach appropriate for the individual patient. Topics reviewed include pharmacotherapy, including opioid management, interventional procedures such as epidural and peripheral nerve catheter placement, nerve blocks, neurolytic procedures, as well as implantable devices. Students with questions may contact Dr. Lance Roy or Esther Turner, 919-681-6437. See Course Catalog at dukehub.duke.edu for full course description.

I am interested in learning about anesthesiology. Where do I start?
ANESTH 220C and/or 440C give a great introduction to and overview of clinical anesthesia, along with exposure to great teaching and amazing residents/faculty. See the “Resources/Education” tab for more details. Subscribe to the listserv to stay up to date on informational and educational events, and look out for announcements regarding the yearly kick-off event and mixer.
What can I do to get involved?
Please feel free to contact the mentors and faculty listed under “Mentors/Anesthesiology Shadowing” for shadowing opportunities in any of the many subspecialties. Reach out to the AIG leadership (contact info above) if you need help getting started, or if you’re interested in helping to lead AIG in future years.