
Fellowship Director
Duke University Medical Center is one of the leading medical centers in the nation with a worldwide reputation for excellence in clinical care, teaching and research. Duke Anesthesiology’s Pain Medicine Fellowship is an ACGME accredited training program. Fellows who successfully complete the program are eligible to sit for board certification.
The fellows spend time at four clinical sites: Duke Pain Medicine clinic, Duke University Hospital, Davis Ambulatory Surgery Center, and the Durham Veterans Affairs Medical Center Pain Clinic. The clinical schedule is designed to provide a broad exposure to pain management in a variety of health care systems so that graduates are well trained to practice independently upon graduation in academic, government or private practice settings.
The Duke Pain Medicine Fellowship prides itself on being a multidisciplinary fellowship and reviews applications from all qualified applicants irrespective of primary specialty. We have trainees and faculty from all ACGME approved disciplines, including anesthesiology, neurology, psychiatry, and physical medicine and rehabilitation. We are particularly looking for self-motivated individuals interested in academic careers.
Follow us on Twitter:
#duekanesfellows_pain
#dukepainfellowship
The Duke Pain Medicine Fellowship accepts electronic applications through ERAS. Once applicants have been interviewed, we participate in the Match.
To be considered for a Pain Medicine Fellowship position:
- Visit https://students-residents.aamc.org/training-residency-fellowship/applying-fellowships-eras/
- Complete application items as instructed by ERAS.
- Include USMLE transcript, Medical School Transcript, Personal Statement, MSPE, and three letters of recommendation.
- Submit In Training Exam scores to anesthes-fellowship@duke.edu.
Important dates for the fellowship application and match process:
- Fellowship applicant registration begins December 1st
- Last day for accepting applications is March 1st
- Fellowship applicants apply to the program through ERAS
- Applicants selected to interview will be notified on a rolling basis beginning late March
- Interviews will be offered May – June
- The deadline for rank list submission and the Match date can be found on www.nrmp.org.
Supplemental application materials may be submitted by email to anesthes-fellowship@duke.edu.

Peter Yi, MD, MSEd
Director, Pain Medicine Fellowship
Assistant Professor
Department of Anesthesiology
Duke University Medical Center
DUMC 3094
Durham, NC 27710
Email: peter.yi@duke.edu
The Pain Medicine Fellowship designs each rotation to expose fellows to a different aspect of pain management. At the Duke Pain Medicine clinic, fellows learn outpatient management under the direction of board certified pain physicians with expertise in procedural intervention and comprehensive management. Special emphasis is given to interventional pain management and procedural competency during the fellowship year.
The fellows additionally spend time at Duke University Hospital on inpatient rotations. They have the opportunity to learn about acute pain management as well as management of chronic pain in the context of acute medical illness. During this time, they also round with the Palliative Care Service and Radiology.
The VA Pain Clinic has been in operation since 1988. It is the third longest-running pain clinic within the Veterans Health Administration System. While at the VAMC, fellows learn a variety of interventional and non-interventional pain management techniques in both the inpatient and outpatient setting. Also at the VAMC, fellows have their Physical Medicine and Rehabilitation rotation.
Rotations
Duke Pain Clinic/Davis Ambulatory Surgery Center/Duke Ambulatory Surgery Center
The Duke Pain Medicine clinic rotation provides exposure to our multidisciplinary pain clinic. At this single location, we have pain psychology, pain psychiatry and physical therapy. Fellows will have an opportunity to work with all the other services provided within the Duke Pain Medicine clinic. Fellows both perform procedures and conduct clinic visits with the Duke Pain Medicine attendings. Procedure days are both in the on-site fluoroscopy suite and at the nearby Davis Ambulatory Surgery Center (DASC). We perform permanent implantation of spinal cord and dorsal root ganglion stimulators, intrathecal pumps, and peripheral nerve stimulators at DASC. Fellows perform vertebral augmentation procedures at the Duke ASC as well. This is a clinic where you hone the skills that will prepare you to be a provider in the private practice or academic setting. Supervision of residents and medical students is another important part of the experience.
Expectations:
- Participate in patient care at the Duke Pain Medicine clinic and Davis Ambulatory Surgery Center
- The first patient is scheduled at 8 a.m. The last patient is typically scheduled no later than 3:40 p.m.
- Supervise medical student interviews and teach physical exam skills
- Formulate differential diagnoses and treatment plans that include both medication management and procedural intervention
- There are no call responsibilities during this rotation
Features:
- Extensive stimulator trial and permanent placement experience
- Multidisciplinary setting
- Fluoroscopically and ultrasound-guided procedures
- Involvement in intrathecal drug delivery program, including implantation
Durham Veteran’s Affairs Medical Center
The Durham Veterans Affairs Hospital (DurVA) is an experience where your pain management skills benefit the men and women who have sacrificed for our freedom. This location is a referral center for complex medical problems from Veterans Health Administration facilities in southern Virginia, North Carolina and coastal South Carolina. You work with one attending daily. The workflow at DurVA is such that patients are evaluated and, if procedural intervention is indicated, the intervention is done during the same clinic visit. This applies to both new and return patients. Thus, fellows have the opportunity to perform multiple procedures daily.
Expectations:
- Participate in patient care at the Durham VA Hospital Pain Clinic. The first patient is scheduled at 8 a.m. The last patient is typically scheduled no later than 3:30 p.m.
- Formulate differential diagnoses and treatment plans that include both medication management and procedural intervention
Features:
- Perform daily procedures (range: 3 – 8)
- Fluoroscopy-guided and ultrasound-guided procedures
- There are no call responsibilities during this rotation
Inpatient Pain Service
The rich acute pain experience at Duke University Hospital provides fellows an opportunity to learn how to manage an Inpatient Pain Service. As part of the “perioperative home” movement that is currently reshaping the field of anesthesia, rotating on the Inpatient Pain Service provides our fellows with a superior training background if they wish to continue practicing inpatient medicine. This service receives consults for acute-on-chronic pain, cancer pain and palliative care.
Features:
- Experience with cancer pain population
- Management of acute-on-chronic pain
- Inpatient setting
Expectations:
- Lead a team of nurses, nurse practitioners, residents, interns and medical students to evaluate and treat acute and acute-on-chronic pain patients
- At-home backup call for inpatient consults during the week. Bi-monthly (1 in 8) Sunday coverage of the inpatient acute and chronic services (shared with Acute Pain and Regional Anesthesia fellows)
- Provide education to the house staff and medical students on the service
Didactics
Didactic sessions include journal clubs, morbidity and mortality conferences, weekly divisional fellow lectures, and weekly departmental fellow lectures. Fellows will present as part of the journal club and M&M conferences.
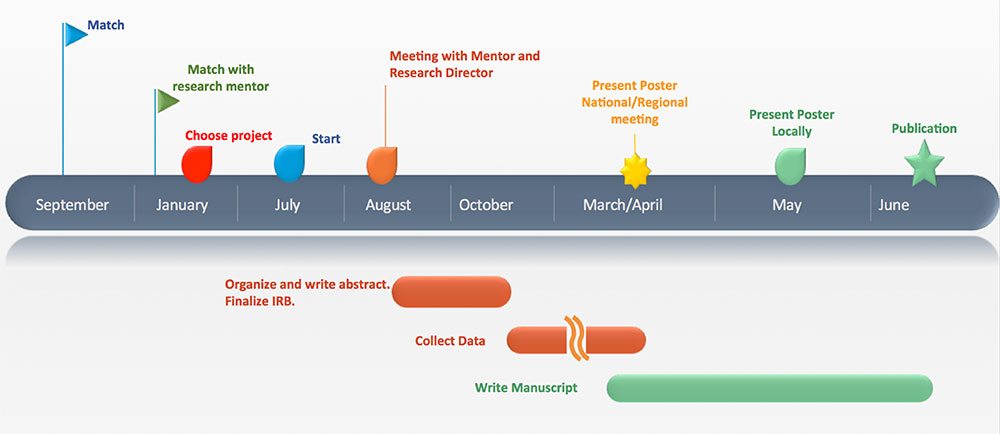
Research Process and Timeline:
Key parts of the 12-month fellowship experience include completion of research. A proposed timeline for fellows who are interested in starting his/her own project:
Fellows have the opportunity to work with faculty members from the renowned Duke Center for Translation Pain Medicine.
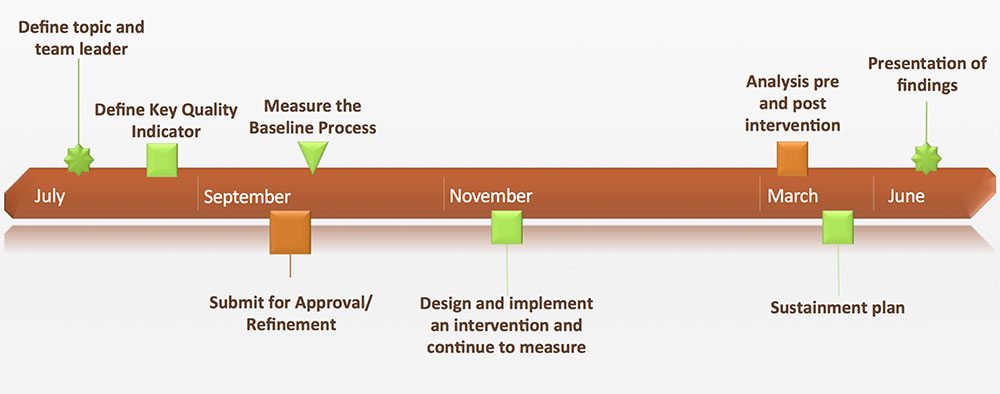
QI Curriculum:
Evaluation:
The Clinical Competency Committee directs all aspects of fellow evaluations and promotion. Dr. Cain Dimon, immediate past fellowship director, chairs the committee. Assessment of progression in ACGME core competencies and milestones are emphasized.
Case exposure includes:
- Traditional spinal cord stimulator
- Dorsal root ganglion spinal cord stimulator
- Kyphoplasty
- InterStim sacral stimulation
- Peripheral nerve stimulation
- Facet and medial branch injections
- Radiofrequency lesioning
- Epidural steroid Injections
- Ultrasound-guided peripheral nerve blocks
- Sympathetic blocks
- Ablative blocks for cancer pain
Additional features of the clinical experience include:
- Ultrasound-guided procedures
- Botox therapy
- Clinical decision making independence
- Management of clinical services
At the completion of the fellowship, successful fellows will have achieved the following goals:
- Obtain independent consultant level of competency in pain management per the ACGME milestones
- Become part of a multidisciplinary team, including nurse practitioners, physician assistants, nurses, residents and medical students
- Safe and skillful management of complicated pain patients, including proficiency in implanted neuromodulation technologies
- Knowledge through organized learning opportunities in a process that is aligned with and complementary to all other aspects of the fellowship requirements
- Knowledge beyond the level expected of a graduating resident in the general areas of pain management
- Understand the tasks, challenges and decisions required of professional colleagues in the areas of pain management (ie: spine surgeons, PM&R, neurologists, psychiatrists, etc.)
- Attain proficiency in intraoperative and postoperative patient management
- Gain expertise in cancer and palliative pain care
Involvement in an anesthesia research project is REQUIRED and assures skill development in:
- Identifying a clinically relevant problem
- Producing a testable hypothesis
- Designing a project to test the hypothesis
- Executing the research project
- Basic statistical methods
- Interpretation of results
- Presentation of results at a regional or national meeting
- Critical evaluation of the literature
Duke Anesthesiology’s Pain Medicine Division has built a true translational research group engaged in innovative pain investigations from bench to bedside and offers multiple world-renowned faculty to provide research mentorship. With the help of a research mentor or mentorship team assigned before the start of the fellowship, each fellow will identify a clinically relevant problem, produce a testable hypothesis and design a project to test that hypothesis. Fellows will also lead a quality improvement project and participate in an institutional patient safety committee.
Fellows interact with residents, interns and medical students on the Inpatient Patient Service and at the Duke Pain Medicine clinic. Teaching opportunities exist within those services. These opportunities include education on physical exam skills, chronic pain and acute pain topics.
Pain management fellows are mentored and taught by faculty from Duke Anesthesiology’s Pain Medicine Division, as well as members of the departments of neurology, physical medicine and rehabilitation, psychiatry, radiology, and palliative care.
After graduation, fellows enter private or academic practice, which varies slightly with each graduating class. To get a first-hand account of our fellowship program, we encourage you to ask our current fellows or alumni about their experiences.
2022-2023
Sameep Baral, MBBS
Andrew Bloomfield, MD
Jacob Byers, MD
Philip Lin, MD
2021-2022
Robert Ackerman, MD
Farooq Anwar, MD
Duran Mitchell, MD, MBA
Matthew Riley, MD
2020-2021
Adam Kemp, MD
Eric Ngo, MD
Anuj Shah, MD
Bharat Sharma, MSc
January 1 – December 31, 2020
Sohan Nagrani, MD
Glenn Nanney, MD
2019-2020
Scott Frieary, DO
Madison Foushee, MD
2018-2019
Osa Emohare, MD
Kyle Fisher, MD
Nenna Nwazota, MD
Jacob Wang, MD
2017-2018
Christopher Davies, MD
Brian Kim, MD
Yoann Millet, MD
Joshua Persaud, MD
2016-2017
Jessica Carter, MD
James Jones, MD
Chad Pletnick, MD
Marc Yeele, MD
2015-2016
M. Yawar Qadri, MD, PhD
Daniel Moyse, MD
Bronwyn Southwell, MD
2014-2015
Matthew Mauck, MD
Timothy Replogle, MD
Nicholas Tinkham, MD
2013-2014
John Holder, MD
Jeffrey Longnion, MD
John Noles, MD
2012-2013
Thomas Hopkins, MD
Hung-Lun John Hsia, MD
2011-2012
Lance Roy, MD
Nam-Kha Pham, MD
2010-2011
Parinaz Azari, MD
Collin Clarke, MD
2009-2010
Dominika James, MD
Daniel Thomas, MD
2008-2009
Davin Mitchell, MD
Takia Oglesby, MD
Michael Lott, MD
2007-2008
Matthew Ranson, MD
Garlon Campbell, MD
Jason Ravanbakht, MD
2006-2007
Kaori Longphre, MD
2005-2006
Peter Nagi, MD
Farrukh Sair, MD
2004-2005
Janice Victor, MD
Shehzad Choudry, MD
Eric Miller, MD
Hsiupei Chen, MD
2003-2004
Hong-Kai Kevin Du, MD
Sonia Pasi, MD
2002-2003
Nadeem Ahmed, MD
2001-2002
Adil Kamal, MD
1998-1999
David Lindsay, MD
1997-1998
Anne Marie Fras, MD
1996-1997
John Haasis, MD
1995-1996
Pam King, MD
1994-1995
Scott Johnson, MD
1992-1993
Toni Harris, MD
The Duke Department of Anesthesiology is committed to cultivating a just and inclusive culture in which individuals thrive and are united in their dedication to alleviating suffering, improving health and well-being, and promoting social justice through excellence in innovation, education, research, service, and professional growth. Learn more about our fellowship programs and Duke Anesthesiology’s Equity, Diversity and Inclusion Program.

Find out why Durham, North Carolina is a great place to work and play.
