The Department of Defense has awarded Duke Anesthesiology’s Paul Wischmeyer, MD, EDIC, FASPEN, FCCM, a four-year $2,203,452 grant for his project titled, “Personalized Targeted Nutrition via StructurEd Nutrition Delivery Pathway to Improve Recovery of Physical Function in Trauma - SeND Home.”
Studies have shown that both military and civilian survivors of trauma suffer significant impairments in physical function, muscle wasting/weakness, and poor quality of life (QoL) post hospital discharge. These impairments, known as ICU-Acquired Weakness (ICU-AW), can affect these patients for months or even years, and have devastating impacts on their personal lives. There are two major drivers of ICU-AW: 1) trauma and critical illness leads to a catabolic state that begins immediately following injury and persists throughout hospital stay, resulting in severe loss of muscle mass and impaired muscle function and 2) many of these patients are significantly malnourished during and after hospital stay. Both civilian trauma patients and injured service members often undergo damage control surgery with multiple abdominal operations spread out over many days; these multiple operations and severe injuries to the gastrointestinal tract often lead to prolonged bowel dysfunction that can significantly delay the initiation of enteral or oral nutrition for a prolonged time, resulting in these patients frequently being made nothing by mouth (NPO) status with a corresponding inability to utilize the intestinal tract.
As a result, less than 50 percent of prescribed nutritional goals are delivered to ICU patients, with surgery and trauma patients often being fed most poorly. A personalized, precision nutrition program for these patients that incorporates early, intravenous, parenteral nutrition (PN) has the potential to reduce muscle wasting and weakness, improve physical function and improve QoL. Precision nutrition care has recently been shown to reduce 30-day mortality, complications, and impaired physical function in non-ICU medical (non-trauma) patients. However, to date, there are no personalized nutrition programs that incorporate the use of indirect calorimetry to target nutritional goals and parenteral nutrition use throughout hospital stay for trauma patients.
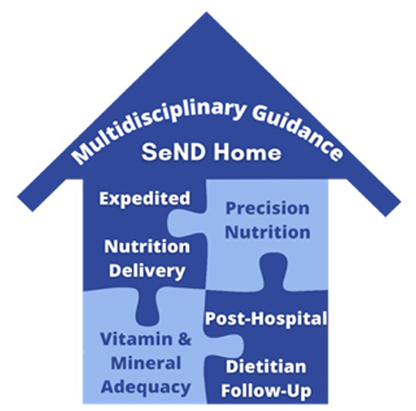
To address this critical need in the field of trauma care, Wischmeyer proposes the first prospective, randomized, phase II clinical trial evaluating their recently developed, personalized, structured nutrition program: the SeND Home Pathway. This pathway includes early total parenteral nutrition guided by indirect calorimetry to precisely target the calorie and energy needs of the patients throughout hospital stay and the enteral and oral nutrition supplements up to two weeks post-hospital discharge. Post-hospital coordination and care is also provided to patients by a registered dietitian for a few months post-discharge. Uniquely, all of these interventions are now possible in forward battlefield hospital settings as well, making early precision nutrition care possible in settings where it was not able to be conducted in the past. Co-investigators include Drs. Krista Haines, Sean Montgomery and Suresh Agarwal of Duke Surgery.
“This study aims to improve physical function and quality of life for veterans and active duty service members, as well as civilian trauma victims, who have suffered severe abdominal injuries requiring extensive surgical procedures,” says Wischmeyer, professor of anesthesiology. “Improvements in the time needed to recover from surgery and to return to duty or one’s desired quality of life will also prevent personnel shortages and reductions in overall military readiness.”