I am truly excited for the opportunity to lead this group of young, bright physicians who shape our identity as a department and community. I look forward to working collaboratively with the residents, department, institution, and our leadership to further drive excellence and growth in our anesthesiology residency program. Together, we will advance the field of anesthesiology and enhance the perioperative experience for patients and their families.
- Brandi A. Bottiger, MD, Residency Program Director
Duke Anesthesiology boasts some of the finest faculty in the country, including worldwide-recognized leaders in anesthesiology practice and research. Our faculty are not only dedicated to recruiting the best and the brightest minds in medicine, they are extremely engaged with resident education and career development. They are a vital component of our nationally-acclaimed Duke Anesthesiology Residency Program which equips our residents with the skills to work with a variety of patient cases and change the world around them, as described by some of our department’s leaders and trainees in the program highlight video (above).
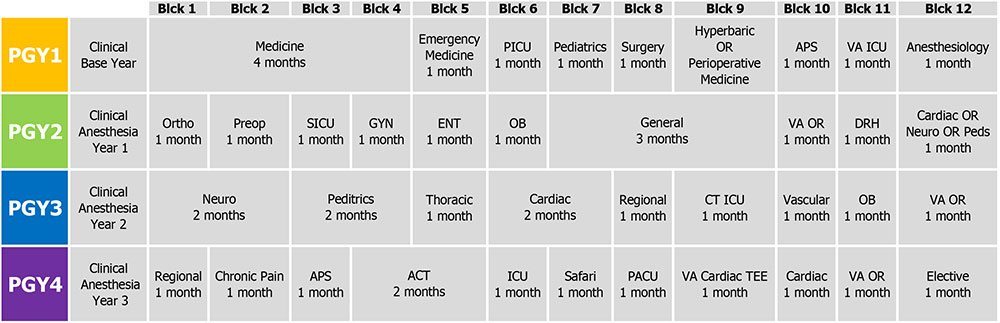
Interns rotate on a variety of services, including Acute Pain Service and Perioperative Medicine, and are able take advantage of the expertise of other Duke departments while developing fundamental clinical skills. CA-1 residents begin building their basic anesthesiology knowledge and start subspecialty training that develops through their CA-2 year. CA-3 residents are able to tailor their final year of training toward their career ambitions and have the opportunity to engage in research projects. In addition to intraoperative and bedside teaching, Duke Anesthesiology offers a strong didactic program for trainees. Each lecture series is organized by faculty leaders to ensure that content is up to date and provides residents the knowledge they need to become world-class anesthesiologists. Trainees have the opportunity to evaluate the lectures and provide feedback to presenters to help ensure the sessions are relevant to the needs of learners. Consequently, our residents are very confident in their ability to work independently in any setting once they graduate from the program.
The Duke Anesthesiology Residency Program’s notable rankings extend beyond our hospital walls and medical campus. Our program offers an exceptional training experience within a vibrant and dynamic community. Durham, often called “The City of Medicine,” is known for its innovation along with its thriving culture, booming culinary scene, athletic spirit, and welcoming college-town atmosphere. It’s a fantastic place to live, grow, and train. Discover more about what makes Durham and Duke special by visiting our “Why Durham?” webpage!
Let's Get Social!

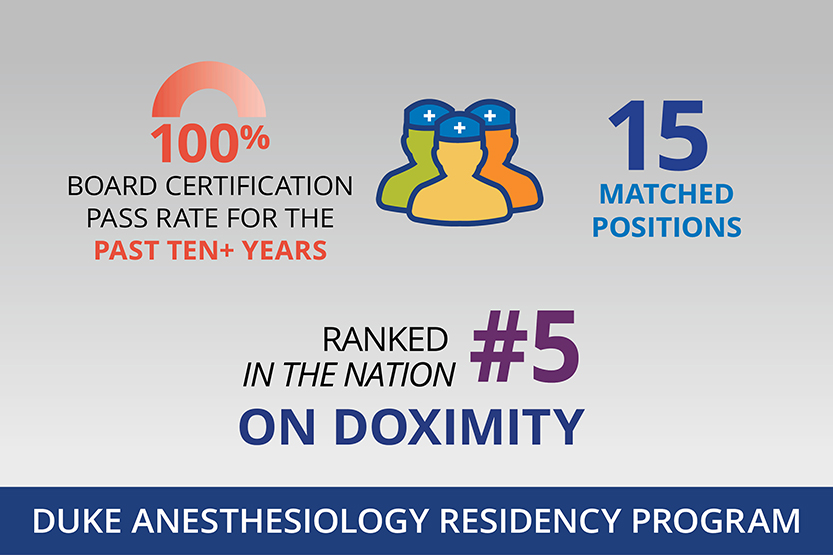
How many positions do you offer?
Typically, we offer 14-15 positions in the Match. One to two positions are reserved for our Academic Career Enrichment Scholars (ACES) Program, a separate NRMP-matched program to support and accelerate the next generation of anesthesiology clinician-scientists. We are approved for a “Reserved” or “R” position; please contact us if you are interested in this position. Applicants may specify any or all tracks when they apply through the Electronic Residency Application Service (ERAS). Interview offers are not based upon applications to a specific track. After applicant interviews, we will determine track preferences. Applicants may declare or change their preferences up until the time that we submit our lists. Information regarding Duke Graduate Medical Education can be found at https://gme.duke.edu.
I am completing a residency currently and am interested in starting as a CA1 in July. Is this possible?
Please contact us with your information.
How do I apply?
We accept applications through the Electronic Residency Application Service (ERAS) and will continue to participate in the National Residency Matching Program (NRMP).
Our application requirements are the same as the standard ERAS application: the complete application, CV, personal statement, medical student performance evaluation (dean’s letter), transcript, and three letters of recommendation. We require Step 1 and Step 2 USMLE scores of all applicants. Step 2 may be completed after the application deadline but must be submitted before ranking in February. Successful completion of USMLE Step 1 and of Step 2 CK is required by Duke University Hospital prior to matriculation.
We abide by the Duke Graduate Medical Education (GME) policy on licensing examinations, with the added stipulation that we require passage of the USMLE Step 3 before starting the CA-1 year.
What tracks do you offer and how many positions?
To complete your ERAS application, you can choose one track or any combination of tracks. For our purposes, these choices are not a binding commitment. If you are invited to interview, you will find out more about each track, and we will ask your track preference before our Match list is submitted.
What are the requirements for international medical graduates?
We have a minimum USMLE cutoff score of 225 on all parts of the exam. IMGs must be ECFMG certified to be considered for an interview. We require some U.S. clinical experience. Observerships do not meet this requirement. We do not have a timeframe for graduation from medical school; we are more interested in what you have done in the time since graduating. Applications are accepted only through ERAS.
I submitted four letters of recommendation. Is that too many?
ERAS allows you to upload up to four letters of recommendation. We consider a complete application to include three letters of recommendation. If you have four, that is fine.
Where can I send questions for the residency program director and assistant directors?
You can submit your questions via email at anesthesiologyresidency@duke.edu.
Other questions?
Please contact us with any questions you may have. You may also refer to the Fellowship and Residency Electronic Interactive Database.
At all levels, leadership, faculty, staff and the residents themselves raise the bar to bring the highest level of dedication and commitment to the Duke Anesthesiology Residency Program.
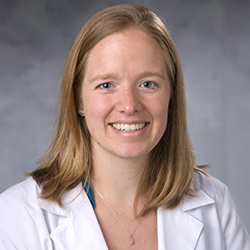
Director, Residency Program
Associate Professor of Anesthesiology
The department welcomed Dr. Brandi Bottiger, associate professor of anesthesiology, to her new role as residency program director in May of 2025. She succeeds Dr. Annemarie Thompson, who was appointed Duke Anesthesiology's vice chair for education in April of 2024 after serving as residency program director for nearly 11 years. As a Duke Anesthesiology alumnus and award-winning educator, Bottiger brings 14 years of experience to her position in which she will lead and mentor approximately 60 future health care leaders within our acclaimed program. For nearly the past decade, she has served as the department’s Adult Cardiothoracic Anesthesiology Fellowship director and in 2019, became the first anesthesiologist to hold a medical directorship position within the transplant center at the Duke University Health System. Bottiger is a visionary leader who will continue to advance the innovative, clinically rigorous, and supportive residency program through robust mentorship and unparalleled clinical and educational experiences.
As Duke Anesthesiology Residency Program alumna, our assistant program directors bring a wealth of firsthand experience and understanding of our program's curriculum and values, and our department's and institution's commitment to excellence. Together, they serve as an integral part of the residency program’s leadership team, assisting with resident advising and mentoring, and enhancement of the clinical and educational environment of the program.
Assistant Residency Program Director
Assistant Professor of Anesthesiology
Angela Pollak, MD, is an assistant professor of anesthesiology in the Cardiothoracic Anesthesiology Division and serves as assistant program director. Dr. Pollak obtained her BA in biochemistry from Washington University in St. Louis and taught in a charter high school serving low-income students in Boston before going on to receive her medical degree from Weill Cornell Medical School in New York. In 2018, Dr. Pollak completed her anesthesiology residency here at Duke in which she served as chief resident. That same year, she was selected to participate in the Feagin Leadership Program, designed to foster the development and training of future academic leaders. She went on to complete Duke’s Adult Cardiothoracic Anesthesiology Fellowship where she served as a chief administrative fellow.
Assistant Residency Program Director
Assistant Professor of Anesthesiology
Sarah Cotter, MD, is an assistant professor of anesthesiology in the Cardiothoracic Anesthesiology Division and serves as assistant program director. Dr. Cotter is an alumna of Duke University. She received her medical degree from the University of North Carolina, Chapel Hill and returned to Duke to complete an anesthesiology residency (Class of 2019) in which she served as a chief resident. That same year, she was selected to participate in the Feagin Leadership Program. Dr. Cotter went on to complete an adult cardiothoracic anesthesiology fellowship at Brigham and Women's Hospital in Boston.
Welcome to the Duke Anesthesiology Residency Program
We’re thrilled you’re considering Duke for your anesthesiology training! Our program offers top-of-the-line clinical experience, strong mentorship, and a vibrant resident community—all in the heart of Durham, North Carolina.
World-Class Clinical Training
As a resident, you’ll primarily train at Duke University Hospital, a Level 1 trauma center, with additional rotations at Duke Regional Hospital and the Durham VA Medical Center. You'll care for complex, high-acuity patients while gaining experience in diverse settings—from academic to community care.
Duke offers a categorical residency, so your intern year (PGY-1) focuses on building a strong foundation through rotations in internal medicine, surgery, ICU, cardiology, emergency medicine, and more—including time with our anesthesiology teams in inpatient pain, hyperbaric medicine, and the Preoperative Anesthesia and Surgical Screening (PASS) clinic.
Alongside your clinical training, you will have access to central anesthesiology texts and several question banks, structured faculty mentorship, didactics oriented towards boards content each year, oral boards prep, and simulation.
Seamless Transition to Anesthesia
After intern year, you'll jump into a 3-week OR orientation alongside your co-residents, guided by senior residents, fellows, and faculty. You’ll be paired up with a fellow intern and guided through OR anesthesia by a dedicated faculty member. Starting July 1 of CA-1, you'll be ready to start managing your own cases—with plenty of support every step of the way. You'll build a strong foundation in anesthesia through a wide variety of cases, including general, colorectal, GYN, ortho, obstetric, and ENT.
Advanced Subspecialty Rotations
In CA-2 year, you’ll take on more complex cases and complete subspecialty rotations in:
- Cardiothoracic Anesthesiology
- Critical Care
- Pediatric Anesthesiology
- Neuroanesthesiology
- Regional Anesthesiology
- Vascular Anesthesiology
- Pain Medicine
You’ll also gain hands-on experience with major organ transplants, including liver, lung, and heart. Most residents meet graduation case requirements by the end of this year—and many begin applying to jobs and fellowships, both at Duke and across the country.
Leadership Development
Your CA-3 year is all about leadership and autonomy. You’ll manage ORs, take senior call, supervise junior residents and CRNAs, and lead clinical teams. You’ll also have several months of elective time to focus on subspecialty interests, global health, research, or career prep.
Faculty & Mentorship
Our program is led by Dr. Brandi Bottiger and a dedicated leadership team that values resident feedback and continuous improvement. Duke faculty are highly-accomplished educators, researchers, and mentors committed to supporting your professional growth in clinical care, education, research, global health care, and quality improvement. Residents also receive funding for presentations at academic conferences.
Life in Durham
Durham offers a fantastic quality of life. Enjoy award-winning restaurants, breweries, Durham Bulls baseball games, and live performances at DPAC. Outdoor lovers will appreciate the nearby parks, hiking trails and greenways, and easy access to both mountains and beaches. With Durham being a small southern city, we enjoy low traffic and better cost of living than most of the country. With Raleigh and our international RDU Airport just 30 minutes away, it’s easy to travel abroad or explore locally in North Carolina.
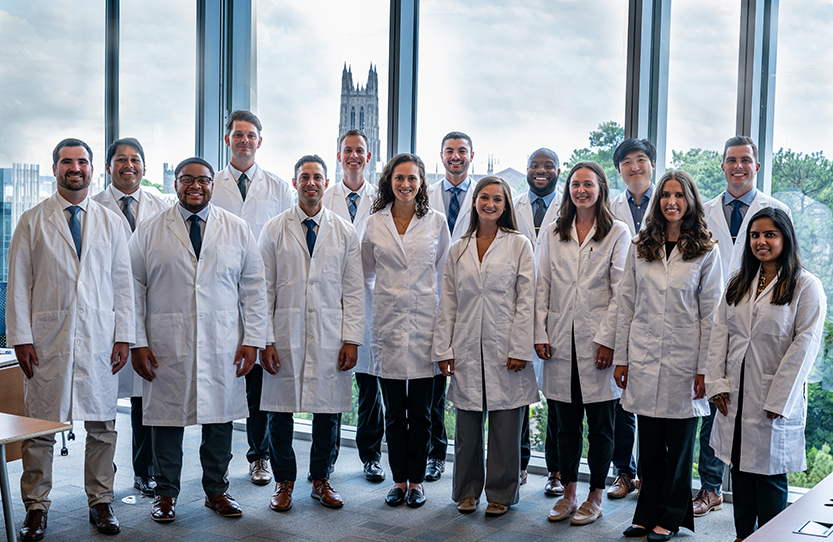
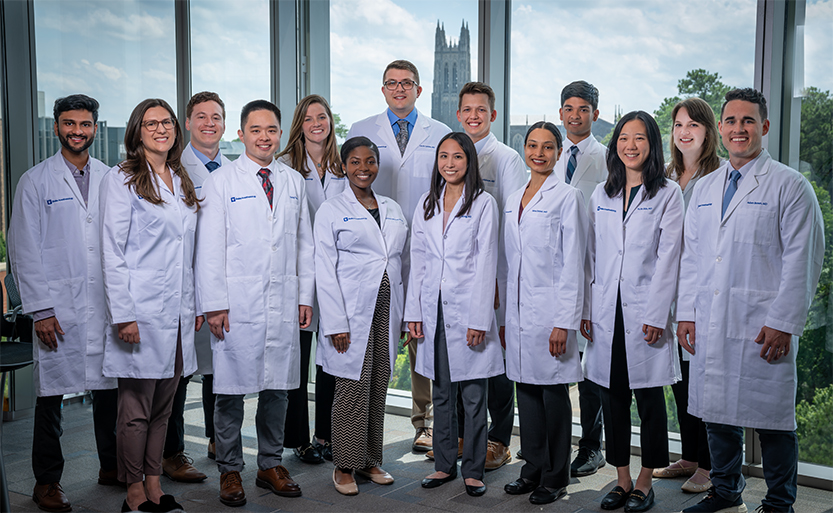
A Diverse, Tight-Knit Community
Our cohort of 60 residents represent a wide spectrum of personal and professional backgrounds and bring a wealth of interests and experiences—runners, musicians, gamers, parents, researchers, and more. We are united by an environment that prioritizes a supportive community and collaborative success. Whether relaxing at a local brewery or swapping stories in the resident lounge, we genuinely enjoy spending time together—both in and out of the hospital.
We hope you’ll take a closer look at Duke Anesthesiology. If you're seeking top-tier training in a welcoming and collaborative environment, we’d love to meet you!
Cheers!
Natasha Navejar, MD | natasha.navejar@duke.edu
Theresa Rizk, MD | theresa.rizk@duke.edu
Where in the World…Are Our Residents From?
The Duke Anesthesiology Residency Program offers a wide variety of learning experiences and resources for trainees including didactics, simulation, and more. This page provides an overview of the resources and educational opportunities available to residents during their four years at Duke.
Residency Didactics
In addition to intraoperative and bedside teaching, Duke Anesthesiology offers a strong didactic program for trainees. Each lecture series is organized by faculty leaders to ensure that content is up to date and provides residents the knowledge they need to become world-class anesthesiologists. Trainees have the opportunity to evaluate the lectures and provide feedback to presenters to help ensure the sessions are relevant to the needs of learners.
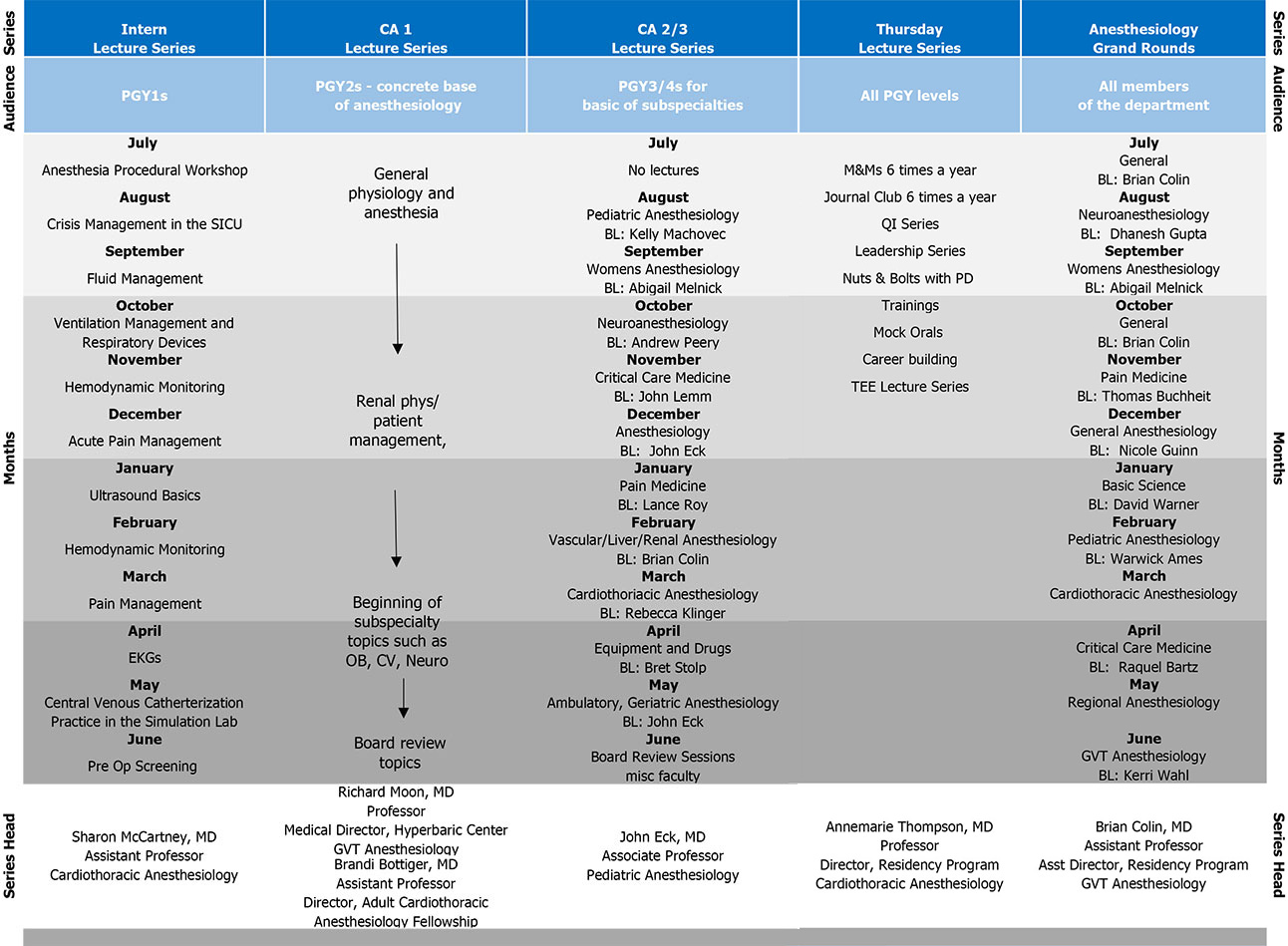
ACGME Anesthesiology Core Requirements: IV A 3: The curriculum must contain didactic instruction through a variety of learning opportunities occurring in a conference setting, in the clinical setting, or online that encompasses clinical anesthesiology and related areas of basic science. Other topics from Internal Medicine that are important for the preoperative preparation of the patient, from surgery as to the nature of the surgical procedure affecting anesthetic care, and from obstetrics that impacts anesthetic management of the patient should be included. The material covered in the didactic program must demonstrate appropriate continuity and sequencing to ensure that residents are ultimately exposed to all subjects at regularly held learning exercises.
Intern Lecture Series
The goal of the intern lecture series is to introduce interns to anesthesiology fundamentals at the beginning of their anesthesiology training. Topics include pre-operative screening, pain management, and ultrasound basics, among others. Lunch is provided for this series that meets once a month on Thursdays from noon to 1:00 p.m.
CA1 Lecture Series: Anesthesiology Fundamentals
This series is designed to build on the intern lecture series by providing trainees a concrete base of anesthesiology as they begin their anesthesiology rotations. Three primary topics are covered over the year:
- General cardio-pulmonary physiology and management
- Renal, hematologic, gastrointestinal and endocrine physiology
- Basics of intraoperative anesthesia management and introductions to subspecialty anesthesia topics (OB, CV, and neuro)
The final portion of the series is devoted to board review topics. This series meets on Tuesday afternoons from 5 – 6 p.m.
CA 2/3 Lecture Series: Subspecialty Anesthesiology
This lecture series is a two-year curriculum that provides advanced residents with in-depth knowledge of anesthesiology subspecialties. Many of these sessions are taught using novel methodologies, including flipped classroom, games, peer-to-peer learning, and case-based discussions.
For many sessions, pre-work is posted online in our course management system. During the live session, residents will participate in active learning activities such as case-based learning, large and small group discussions, and review games in a “Jeopardy” format. This series meets on Wednesdays from 5 – 6 p.m.
All Residents Lecture Series: Thursday Series
The Thursday afternoon lecture series is designed to provide trainees with the knowledge and skills they need to succeed as well-rounded attending anesthesiologists post-training. This series focuses on the following ACGME competencies: practice-based learning and improvement, interpersonal and communication skills, and systems-based practice. During the course of the year, residents will participate in the following activities on Thursday afternoons from 5 – 6 p.m.:
- M&Ms (6x/year)
- Twitter Journal Club (3x/year)
- QI lectures
- Nuts and bolts meetings with residency program leadership
- Leadership development sessions
- Mock orals
- TEE Interactive Series (see TEE below).
Resident TEE Curriculum
The Resident TEE curriculum is a 6-month curriculum for CA-2 and CA-3 residents focused on basic perioperative TEE; including image optimization, recognition of valvular abnormalities, ventricular dysfunction, and hands-on image acquisition.
Simulation
In addition to didactics, Duke Anesthesiology trainees have the opportunity to participate in world-class simulation activities. These sessions use various modalities of simulation, including task trainers for procedural skills as well as high-fidelity mannequins for case-based scenarios. A faculty champion, often division-specific, leads each session. The curriculum is developed and standardized in collaboration with simulation staff to ensure a paramount learning experience for all participants. The chart below reflects simulation-based education for graduate medical education in the Department of Anesthesiology.
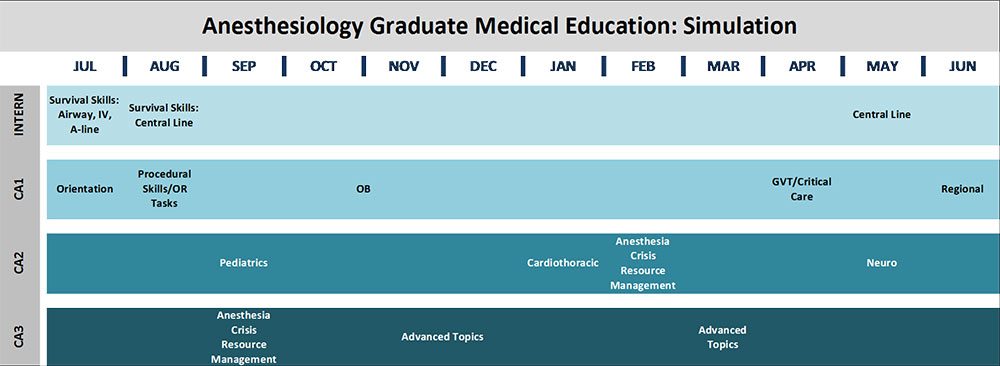
Intern Survival Skills: Procedure-based simulation training including central line, airway management, and IV placement led by Dr. Sharon McCartney.
Subspecialty Case-based Scenarios: Organized by Dr. John Eck, these regular sessions rotate CA-1, CA-2, and CA-3 learners through cases created by champions in each subspecialty.
Anesthesia Crisis Resource Management (ACRM): Complex case-based scenarios that challenge CA-2 and CA-3 learners with crisis resource management-focused debriefings. The course originated with Dr. Ankeet Udani.
Education Highway
Trainees have access to the Education Highway, an online departmental repository for learning materials. This tool provides opportunities for self-directed learning in addition to supporting the flipped lectures. Each division has a space, curated by a faculty member with expertise in that area, to house educational videos, significant papers, protocols, and other learning materials. Each week, a recording of the departmental Grand Rounds lecture is posted for viewing by those unable to attend.
Advising and Coaching
Each resident has the opportunity to choose a faculty adviser. In addition to the support provided by the resident’s adviser and residency program leadership, the department’s PhD educator, Ashley Grantham, is also available for individual educational coaching.
Other Resources
The following individuals are available to answer questions about the educational opportunities available in the department for trainees:
Brandi A. Bottiger, MD
Director, Anesthesiology Residency Program
Associate Professor of Anesthesiology
Angela Pollak, MD
Assistant Director, Anesthesiology Residency Program
Assistant Professor of Anesthesiology
Sarah Cotter, MD
Assistant Director, Anesthesiology Residency Program
Assistant Professor of Anesthesiology

Residents in the Duke University Department of Anesthesiology have endless opportunities to involve themselves in research. All subspecialty divisions within the department are academically productive, with nearly all research faculty actively managing multiple simultaneous projects. For those interested in basic science, our division boasts several productive laboratories investigating pain, myocardial ischemia/reperfusion injury, neuroprotection, and the role of G-protein coupled receptors in human disease.
The Department of Anesthesiology is also fortunate to have unparalleled support for clinical research (Clinical Research Unit or CRU), allowing straightforward design and conduct of complex and unique clinical investigations. While participation in research is not required, resident research collaboration is both important and universally appreciated by investigators. Residents are encouraged to attend research meetings when their training schedule allows. Furthermore, residents presenting at national meetings typically receive departmental financial support for travel, board, meals, and attendance. For residents who are interested in a research-focused career, the residency training program offers two ACES positions annually. Please refer to the ACES program section of the website for more information.
Mandatory Rotations
| Department | Rotation | Location |
|---|---|---|
| Anesthesiology 2-3 months |
Clinical Anesthesiology Acute Pain Service Perioperative Medicine |
DUMC DUMC DUMC |
| Medicine 4-5 months |
General Medicine Cardiology Cardiology Consults Hyperbaric & Undersea Medicine* Pulmonary Medicine |
DRH DUMC DUMC DUMC DUMC |
| Emergency Department 1 month |
Emergency Medicine | DUMC |
| Pediatrics 1-2 months |
General Pediatric Wards Pediatric ICU |
DUMC DUMC |
| Surgery 2 months |
Surgical ICU* General Surgery |
VA DRH |
*Managed by the Department of Anesthesiology
DUMC=Duke University Medical Center
DRH=Duke Regional Hospital
VA=Durham Veterans Affairs Medical Center
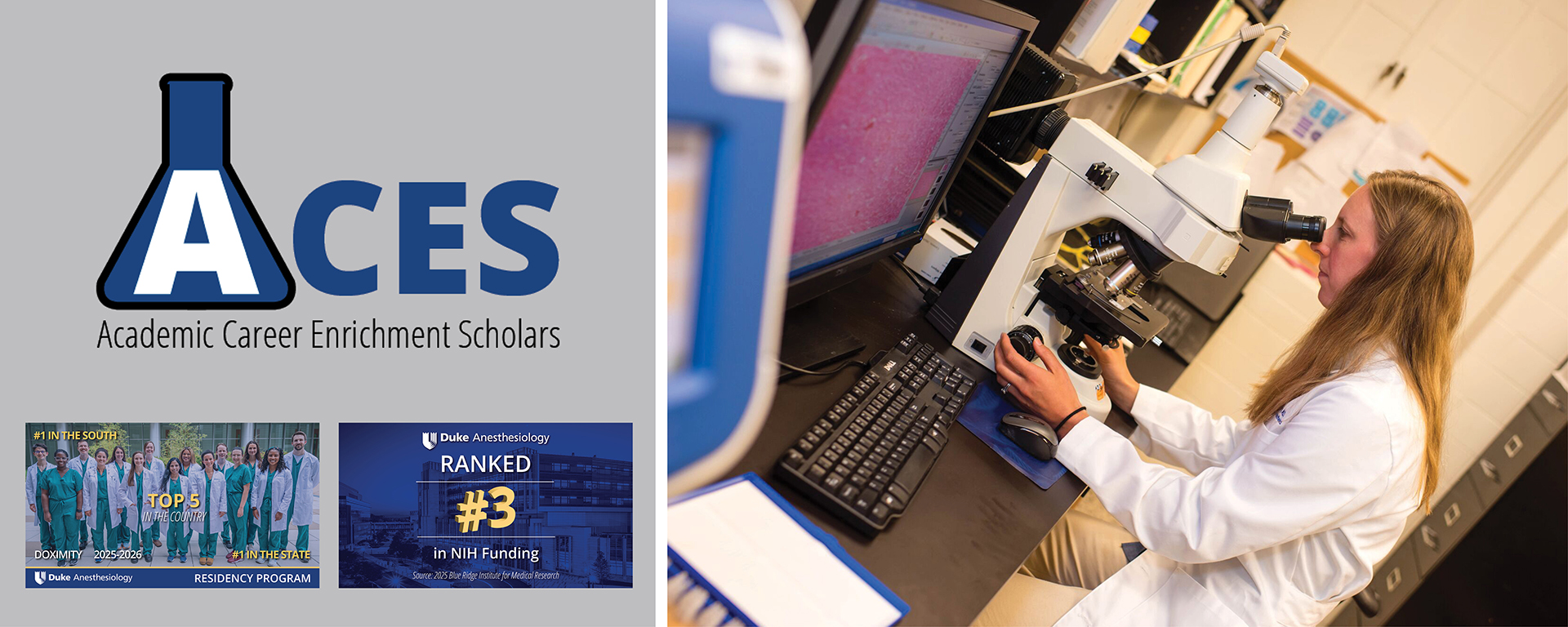
Duke Anesthesiology created the Academic Career Enrichment Scholars (ACES) Program in 2007 to integrate advanced clinical and research training without prolonging the duration of the traditional residency and fellowship system. This innovative curriculum program is a highly-selective resident research track designed to increase the number of graduates pursuing academic careers and help them gain status as independently-funded researchers. It matches up to two residents per year. Since 2007, 24 trainees have graduated from the ACES Program or are currently in the program. To date, ACES residents have brought in more than $27 million in extramural funding, have published more than 450 peer-reviewed papers, and 22 of 24 graduates (91%) remain in academic anesthesiology.
Bella Vishnevsky, MD
Regional Anesthesiology and Acute Pain Medicine Fellow
Megan Fah, MD
Critical Care Medicine Fellow
Leah Acker, MD, PhD
CA-3 / ACES Chief Resident
Katherine Sun, MD
CA-2 Resident
Bryan Chow, MD
CA-3 Resident
Reade Tillman, MD
CA-2 Resident
Suhas Kochat, MD, MBA
CA-2 Resident
John Ward, MD
CA-1 Resident
Bella Vishnevsky, MD
Regional Anesthesiology and Acute Pain Medicine Fellow
Emily Barney, MD
CA-1 Resident
Yohannes C. Constable, MD
CA-3 Resident
Michael Cutrone, DO
Adult Cardiothoracic Anesthesiology Fellow
Kathryn Pearson, MD
CA-2 Resident
Henry Lather, MD
CA-3 Resident
Leah Acker, MD
CA-3 / ACES Chief Resident

Find out why Durham, North Carolina is a great place to work and play.

Resident Classes of 2025-2026
Interns
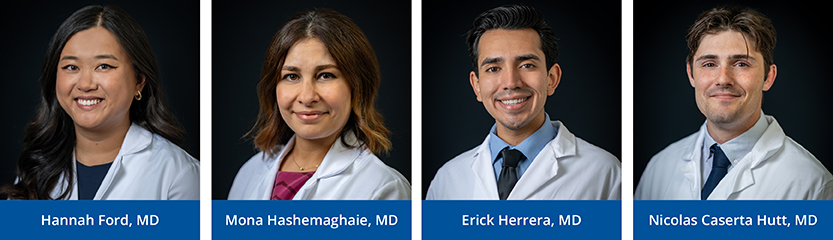
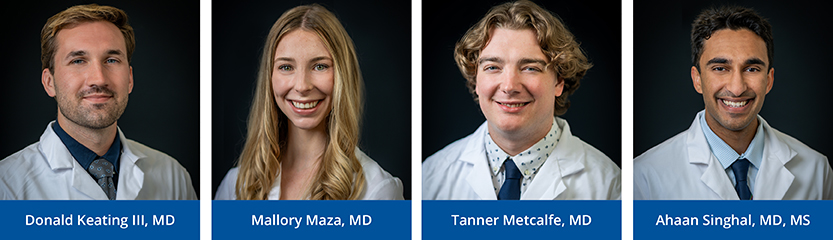

CA-1s
CA-2s
CA-3s
Residency Program Class of 2025