Mary Yurashevich, MD, MPH, MHSc
Thank you for your interest in the Obstetric Anesthesiology Fellowship program at Duke University Hospital. We have trained fellows for 20 years and have maintained ACGME-accreditation since its inception in 2012. In 2019, we were recognized by the Society for Obstetric Anesthesia and Perinatology as a “SOAP Center of Excellence”.
Duke Anesthesiology offers two positions per year for a one-year, ACGME-accredited fellowship in obstetric anesthesiology. The Duke University Birthing Center is the primary clinical site for OB anesthesia fellows; it is a Level 3 regional referral center with approximately 4,200 deliveries per year that encompass a range of maternal and fetal conditions. Fellows manage the care of parturients with high-risk fetal conditions including those needing fetal surgery, that are referred to the Duke Intensive Care Nursery, a 50-bed, Level IV neonatal intensive care nursery.
2027-28 Obstetric Anesthesia Fellowship Application cycle:
Duke will be participating in the SF Match for Obstetric Anesthesia Fellowship positions, sponsored by the Society for Obstetric Anesthesia and Perinatology.
All interviews will be conducted virtually.
We remain an ACGME-accredited program and will accept applications for the 2025-26 fellowship year through SF Match starting in January 2025.
To be considered for an obstetric anesthesiology fellowship position, please register and submit your application through SF Match.
Applicants interested in a 2-year combined fellowship at Duke should e-mail Dr. Yurashevich directly to inquire: mary.yurashevich@duke.edu.
Important Dates for the 2027-2028 Fellowship Application and Match Process:
- January 2026: Applicant Registration Begins
- February - April 2026: Interviews Offered
- June 9, 2026: Rank List Due
- June 16, 2026: Match Day!
Questions and concerns can be directed to anesthes-fellowship@duke.edu.
Mary Yurashevich, MD, MPH, MHSc
Associate Professor
Fellowship Program Director
Division of Women’s Anesthesia
Department of Anesthesiology
Duke University Medical Center
DUMC 3094, Durham, NC 27710
Email: mary.yurashevich@duke.edu
| ROTATION | DURATION |
|---|---|
| Labor & Delivery | 7 months |
| Research | 3 months* |
| Maternal-Fetal Medicine | 2 weeks |
| Neonatology | 2 weeks |
*1-2 dedicated research days/week during each rotation
Labor & Delivery Rotation
Clinical:
For seven months, an OB anesthesia fellow actively leads the OB anesthesia team, which includes residents and a nurse anesthetist. The fellow leads the twice-daily handover rounds with MFM, in addition to consulting with obstetric colleagues throughout the workday. During the second half of the training year, the fellow takes a limited amount of overnight calls with a resident; the OB anesthesia attending is available in-house for consultation. OB anesthesiology fellows lead the pre-operative planning and multi-disciplinary collaboration for the care of high-risk parturients, and are involved in the majority of these cases with the support of a faculty member.
Didactics and Conferences:
- Obstetric Anesthesia Lecture series: Regular, planned lectures on a range of topics pertinent to an advanced consultant in obstetric anesthesia that are recommended by ACGME and taught by obstetric anesthesiology faculty members, as well as MFM and neonatology faculty
- Monthly SOAP-sponsored Virtual Obstetric Anesthesiology Grand Rounds will be watched with a faculty member in order to facilitate discussion
- Journal clubs: fellows will prepare and present articles for journal clubs during the fellowship year, including a joint-MFM journal club
- Morbidity and mortality conferences in anesthesiology & obstetrics
- Weekly multidisciplinary conferences — high-risk antepartum patients
- Monthly, multidisciplinary conferences — high-risk fetal patients
- Fetal Heart Rate monitoring interpretation course – MFM faculty
- Weekly Departmental Fellowship Seminar series: Aimed at issues of general interest to the anesthesiologist including professionalism, leadership, business management, education, career development, ethics, oral board preparation, and numerous other topics. These sessions are led by departmental faculty.
- Quality & Safety Course: Taught by anesthesiology faculty experts in quality improvement and patient safety. Course is taken in conjunction with other departmental fellows. Fellows develop their own QI project.
- Transthoracic Echocardiography Workshops: Taught by board-certified, echocardiography experts from the Division of Cardiothoracic Anesthesiology. This is an excellent opportunity to learn basic TTE examination skills and how they can be used to optimize the care of critically ill parturient.
- Advanced Crisis Resource Management training and leadership development in our state-of-the-art Duke Human Simulation & Patient Safety Center. Opportunity to participate in multi-disciplinary obstetric emergency simulations with obstetricians, anesthesiologists and nurses.
- Point of Care Ultrasound Certification (Optional): Fellows that choose to pursue the POCUS elective will participate in a structured curriculum that adheres to training guidelines endorsed by all three U.S. critical care societies (SCCM, ACCP, ATS). POCUS training will cover the following organ systems: focused cardiac; focused pleural/pulmonary; focused renal/GU; focused DVT; and FAST exam.
Maternal-Fetal Medicine Rotation
The OB anesthesia fellow will join their MFM colleagues for a two-week, in-depth look into their practice and antenatal considerations of patient care. The OB anesthesia fellow will attend morning rounds with the antepartum inpatient team, as well as outpatient clinics including the Duke Fetal Diagnostic Clinic and high-risk obstetrics clinics. The MFM faculty actively engage our fellow in educational topics best explained by them, in addition to seeking the anesthesia perspective on care considerations for high-risk patients.
Neonatology Rotation
The OB anesthesia fellow will rotate for two weeks in the Duke Intensive Care Nursery (ICN). This ACGME-required rotation is organized and led by Dr. Susan Izatt. The OB anesthesia fellow will attend morning rounds with the ICN team, as well as all cesarean deliveries as an active member of the neonatal resuscitation team. This two-week experience provides additional insight into the neonatal impact of antenatal and perinatal decisions, and has proved to be exceptionally valuable for our fellows. After completing this rotation, fellows will receive Neonatal Resuscitation Program™ certification.
International Maternal & Child Health (Optional Rotation)
Several of our Duke OB Anesthesia faculty are actively involved with Kybele, an international, non-profit organization devoted to the reduction of maternal morbidity and mortality worldwide. Their participation with this organization allows them to contribute to the improvement of maternal health through clinical, educational and research activities in other countries. This relationship also provides an opportunity for our fellows and residents to extend research projects to other practice sites, such as Ridge Regional Obstetric Hospital in Accra, Ghana. Read more about past OB Anesthesia fellows’ experiences in Ghana.
The Division of Women’s Anesthesiology currently has eleven faculty members who subspecialize in obstetric anesthesiology and provide 24 hour/day, on-site coverage for the Duke Birthing Center. In addition to dedicated teaching from Division of Women’s Anesthesiology faculty, fellows rotate with, and receive ongoing teaching from, faculty in Maternal-Fetal Medicine (MFM) and Neonatology. MFM attendings also provide 24 hour/day, on-site coverage at the Duke Birthing Center. Fellows are provided a supportive environment in which develop clinical, consultant and in-depth research expertise.
With no more than two fellows per year, our fellowship program has all the advantages of a small program with the resources and patient acuity of a larger program. The small number of OB anesthesiology fellows ensures access to all interesting cases and clinical subjects for research projects. However, OB anesthesiology fellows enjoy opportunities for collaboration, as well as social support, with the more than 30 fellows per year across the nine sub-specialties in the Duke Department of Anesthesiology. The department holds weekly fellows seminars designed to be of broad interest to trainees of all sub-specialties, as well as provide an opportunity for engagement among fellows. This series includes formal education and guidance on the development and completion of a quality improvement project. The Fellows’ Office provides all fellows in the Department of Anesthesiology personal workspace that is conveniently located to clinical worksites. OB anesthesiology fellows also engage regularly with fellows in maternal-fetal medicine through clinical work, joint conferences and journal clubs.
Additional features of our clinical practice include:
- Social, economically and ethnically diverse patient population
- 40 percent cesarean section rate
- 90 percent neuraxial labor analgesia
- Multi-disciplinary Maternal Hemorrhage Protocol in place for over 10 years
High risk conditions commonly managed:
- Severe preeclampsia & HELLP syndrome
- Referral center for abnormal placentation: multi-disciplinary team approach
- Maternal cardiac disease
- Maternal congenital heart disease
- Pulmonary hypertension
- Respiratory diseases
- Endocrine disorders
- Post-transplant parturients
- Super-morbid obesity
- Oncologic conditions
- HIV
- Polysubstance abuse
- Neurologic conditions.
Fellowship goals include maximizing proficiency in:
- Providing compassionate, culturally-sensitive anesthetic care to both high and low-risk parturients from a diverse range of socio-economic, ethnic and religious backgrounds
- Leading an anesthesia team of anesthesia residents and nurse anesthetists to provide comprehensive peripartum anesthetic care on a high acuity labor and delivery unit in concert with nurses and other physician specialists from maternal-fetal medicine, neonatology, pulmonary, cardiology, surgery, hematology, neurology, transfusion medicine, or interventional radiology
- Demonstrating technical expertise and clinical judgment to perform all neuraxial anesthetics and any medically-indicated invasive monitors, including expertise in the use of ultrasonography for neuraxial placement and cardiac assessment
- Demonstrating competence in the comprehensive analgesic/anesthetic management of both maternal and fetal comorbidities for:
- Vaginal deliveries with high-risk maternal or fetal conditions
- Planned/emergent cesarean deliveries with high-risk maternal or fetal conditions
- Non-obstetric, antepartum surgery
- Antepartum fetal surgery
- Antepartum consultations with high-risk parturients
- Care of the critically-ill parturient and advanced crisis resource management
Other clinical education opportunities include:
Given the resources and collaborative nature of the practice at Duke, arrangements can be made based on specific interest of a fellow to work with physicians in different specialties who are also involved in the care of our pregnant patients. These opportunities include, but are not limited to cardiology, pulmonary and transfusion medicine.
Involvement in an anesthesia research project is REQUIRED and assures skill development in:
- The ability to formulate clinically relevant hypotheses in obstetric anesthesiology and perinatology
- Research design to create achievable studies that will answer questions according to scientific methods
- Execution of research project
- Introduction to statistical analysis techniques
- Interpretation of results and preparation of a manuscript
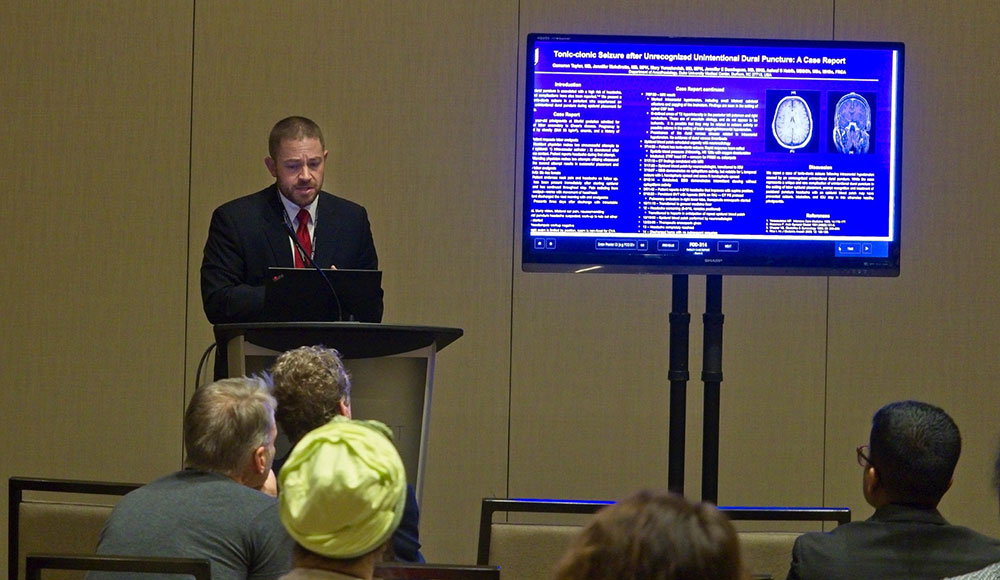
- Presentation of research at national or international meetings, which forms the basis of a peer-reviewed manuscript submission for publication
- Introduction to research funding and grants
- Ability to critically evaluate the research of other investigators
Research opportunities include clinical and basic science research with mentors from anesthesiology and obstetrics. The research interests and publications of Duke faculty can be explored at Scholars@Duke. In addition, Duke has maintained the use of electronic anesthetic records for obstetric patients since 2003, which greatly facilitates retrospective database studies. Duke University Hospital and the Duke Department of Anesthesiology have a vast research infrastructure that supports the research activities of OB anesthesia fellows during the year of training, including scientific writing courses and access to statistical support. Fellows also participate in an institutional patient safety committee and lead a quality improvement project. Fellows are provided with a laptop computer and a $1,500 educational stipend for education or travel to national meetings such as the Society for Obstetric Anesthesia and Perinatology (SOAP). Fellows are strongly encouraged to present abstracts and give lectures at local and national meetings.

OB anesthesia fellows will work closely with Duke Anesthesiology residents and medical students during their rotations on OB anesthesia, and in the management of patients for non-obstetric, antepartum surgery. Fellowship teaching opportunities also include didactic lectures, dedicated obstetric simulation sessions at the Duke Human Simulation and Patient Safety Center, journal clubs, and division M&M. Fellows can also participate in the Duke AHEAD program that provides opportunities to learn and develop teaching skills.
OB anesthesiology fellows are taught and mentored by faculty from the Divisions of Women’s Anesthesiology, Maternal-Fetal Medicine and Neonatology. Meet our faculty and find out what our OB anesthesiology fellowship alumni have been up to!

Find out why Durham, North Carolina is a great place to work and play.