Thank you for your interest in the Regional Anesthesiology and Acute Pain Medicine Fellowship program at Duke University Medical Center. We have been a world-renowned leader in regional anesthesiology training for decades, and in 2017 became one of the first programs in the country to be ACGME accredited in Regional Anesthesiology and Acute Pain Medicine. With a combination of extraordinary clinical experience, a structured educational program, mentoring by world experts, and a strong focus on fellow scholarship and inquiry, our fellows emerge prepared with the tools to make a profound impact at the patient, departmental, health system and national levels.
Our Regional Anesthesiology & Acute Pain Medicine Fellowship Program participates in the SF Match process, under the sponsorship of the American Society of Regional Anesthesia.
To be considered for a Regional Anesthesiology & Acute Pain Medicine fellowship position:
- Visit sfmatch.org to register as an applicant and rank programs
Important Dates for the 2027-2028 Fellowship Application and Match Process:
- January 5, 2026: Applicant Registration Begins on SF Match
- March - April 2026: Interviews Offered (virtual)
- March 31, 2026: Applications Due
- June 1, 2026: Rank Lists Due
- June 8, 2026: Match Day
Applications may be submitted through SF Match. Fellowship questions can be directed to:
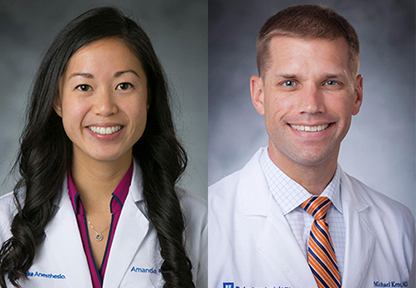
Amanda H. Kumar, MD
Fellowship Program Director
Department of Anesthesiology, Orthopaedics, Plastics, and Regional Division
PO Box 3094 #19
Duke University Medical Center
Durham, NC 27710
Email: amanda.kumar@duke.edu
Michael L. Kent, MD
Associate Program Director
Department of Anesthesiology, Ambulatory Anesthesiology Division
PO Box 3094 #19
Duke University Medical Center
Durham, NC 27710
Email: michael.kent@duke.edu
LuAnne Latta
Program Coordinator
Regional Anesthesiology & Acute Pain Medicine Fellowship
Department of Anesthesiology
Duke University Medical Center
DUMC 3094 #4
Durham, NC 27710
Email: luanne.latta@duke.edu
Phone: 919-681-9941
Fax: 919-668-2081
LyAshia Webb
Program Coordinator
Regional Anesthesiology & Acute Pain Medicine Fellowship
Department of Anesthesiology
Duke University Medical Center
DUMC 3094 #34
Durham, NC 27710
Email: lyashia.webb@duke.edu
Phone: 919-222-2222
Fax: 919-681-8994
Clinical time is spent in the following rotations:
| ROTATION | DURATION |
|---|---|
| Block Area & Operating Room (Duke North) | 20 weeks |
| Block Area & Operating Room (Ambulatory Surgery Centers) | 20 weeks |
| Inpatient Pain Service | 10 weeks |
| Chronic Pain | 2 weeks |
Block Area & Operating Room (Duke North and Ambulatory Surgery Center)
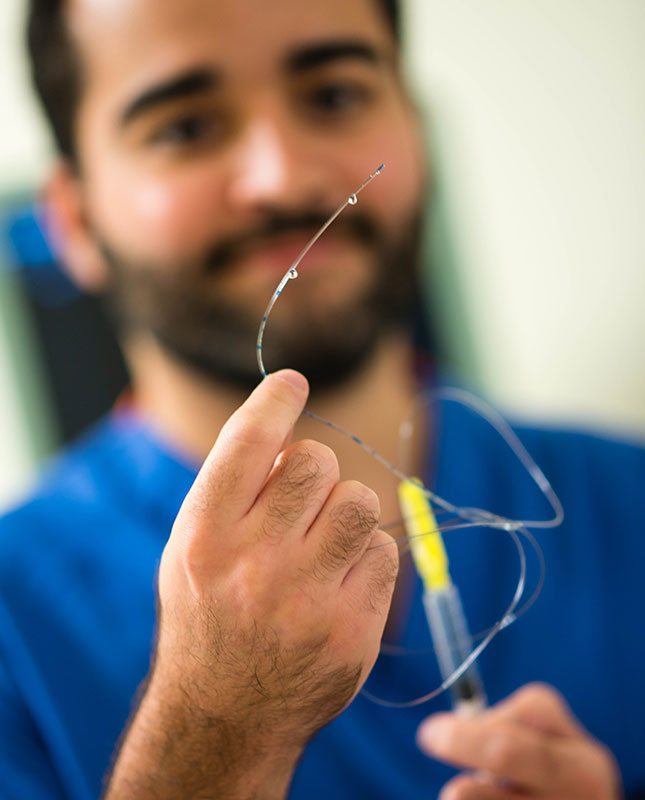
Fellows are assigned to directly care for patients in the operating room 2-3 clinical days per week under the supervision of a RAAPM faculty member. In addition to performing his/her own peripheral and neuraxial blocks under supervision, the fellow has the opportunity to manage these patients throughout the perioperative period. Surgical cases include elective orthopaedic surgery (eg, joint arthroplasty, hand surgery, orthopaedic oncology, and sports medicine) as well as a wide variety of other clinical service lines (eg, trauma, vascular, breast, plastics, spine, etc) to provide our fellows a comprehensive experience.
The remaining clinical days per week are spent in the preoperative block area. Fellows serve as a leader in the block area, performing a variety of peripheral, truncal, and neuraxial blocks for a diverse array of clinical services under the supervision of RAAPM faculty. On a typical day, fellows may perform 10-35 perineural or truncal blocks. Fellows also have the opportunity to lead and teach residents on their regional anesthesia rotations, and serve as consultants for anesthesiology attendings who may request assistance with advanced block procedures (eg, TAP, rectus sheath, external oblique, QL, ESP, interpectoral and pectoserratus, paravertebral, etc). Additionally, fellows may be called on to perform rescue blocks in the Emergency Department and PACU.
This rotation is split between our main hospital (Duke North, a tertiary level 1 trauma center) and our Ambulatory Surgery Centers. This is designed to expose fellows to the complete breadth and depth of regional anesthesiology clinical practice. Whether caring for elite athletes in the fast-paced ambulatory sports medicine rooms, placing multiple catheters for lower limb amputation, or choosing just the right combination of blocks for a patient undergoing mastectomy and reconstruction, one of the foundational goals of our fellowship is to ensure that there is no clinical scenario, technique or judgment call relating to acute pain medicine and regional anesthesiology that our fellows have not faced as they prepare for their roles as leaders in the field.
Skill in the use of ultrasonography is acquired throughout the academic year. In addition to the techniques related to regional nerve blocks, fellows receive instruction in Point of Care Ultrasonography (POCUS), including transthoracic echocardiography, gastric, lung, and IVC ultrasound.

Inpatient Pain Service (IPS)
Fellows spend a total of 8-10 weeks on the IPS where they assume the leadership role on a team of other trainees and mid-level providers, all under the guidance of acute pain faculty. On this service, the fellow learns to manage acute postoperative pain using a variety of pharmacologic, non-pharmacologic, and nerve block-based techniques and tools. Rounds are conducted daily on a patient population primarily consisting of those with peripheral and neuraxial catheters in situ and those on ketamine or lidocaine infusions. This includes patients on the surgical floors, the critical care units, and the pediatric floors. The management of new acute pain consults and the placement of peripheral nerve or neuraxial blocks is a substantial part of the IPS experience.
Chronic Pain Rotation
Pain doesn’t respect the strict boundaries of “acute” and “chronic” and there is a lot to be gained by managing patients who have longstanding pain needs. Fellows spend two weeks seeing new consults for chronic nonmalignant and cancer pain and using many of the tools learned in the care of acute pain management to help ease the suffering of these patients. This inpatient rotation is done at Duke North.

Structured Educational Program
Much of the learning in regional anesthesiology and acute pain medicine occurs through observation, hands-on instruction and mentored practice at the bedside. However, the RAAPM fellowship at Duke prides itself on a strong foundation of structured learning opportunities. These include:
- Simulation: Duke’s state-of-the-art Human Simulation and Patient Safety Center is internationally recognized for its educational innovation. Fellows participate in multiple high-fidelity simulation courses throughout the year with a particular emphasis on anesthesia crisis resource management of rare, critical scenarios. One simulation course focuses on regional anesthesia and acute pain management, including the diagnosis and management of complications. Another course is a joint simulation course with other anesthesia subspecialty fellows to consolidate both technical and non-technical skills.
- Tuesday Afternoon Seminar Series: Every Tuesday afternoon from 4:30-5:30 pm is protected time for the fellows to take part in a seminar, lecture, or problem-based learning discussion. These sessions are always led by a RAAPM faculty member and tend to focus on topics that are best suited to a discussion or classroom type environment. Examples include:
- Hemorrhagic and infectious complications of regional anesthesia
- Regional anesthesia and pain management for pediatrics
- Opioid pharmacology of methadone, tapentadol, and buprenorphine
- Intravenous regional anesthesia
- The regional anesthesiologist’s perspective on intrathecal pumps and spinal cord stimulators
- Oromaxillofacial, scalp, and airway nerve blocks
- Local anesthetic pharmacology and adjuvants
- Peripheral nerve stimulation and paresthesia nerve localization techniques
- Pharmacogenomics
- Acupuncture
- Setting up an ambulatory surgery center and regional anesthesia service
- Billing practices in regional anesthesia and acute pain management
- Education in regional anesthesia and the role of simulation
- Sonoanatomy Scanning Sessions: These hour-long hands-on sessions run primarily throughout the first half of the fellowship year and are designed to familiarize the fellow with the sonoanatomy of the entire body, with particular emphasis on neurologic, vascular and musculoskeletal structures. Each of the twelve sessions tackles a separate region of the body and focuses on identification of relevant structures to safely perform various peripheral and neuraxial blocks, vascular access procedures, and musculoskeletal diagnostic and interventional procedures.
- Journal Club: Throughout the year, each of the fellows presents a recently published article that is of interest to him/her. The goal of this series is both to acquire skills in critical appraisal of the literature and to educate the group about new and interesting studies. Fellows often select articles that highlight novel or controversial topics and are assigned a faculty mentor to help guide them through the process of evaluating the study methodology. Fellows also participate in journal clubs and educational series with fellows from outside RAAPM fellowships to foster networking and cross-institutional collaboration as well as orthopaedic surgical colleagues.
- Departmental Fellowship Seminar Series: On Monday afternoons, fellows attend an educational lecture series that focuses on more general topics, such as leadership, statistics, quality improvement, or oral board preparation. This affords the fellows an opportunity to learn and discuss these topics with fellows from other anesthesiology subspecialties.
Research
Scholarship and inquiry are part of the foundation of the fellowship. Fellows are trained in research methodology including the generation of a hypothesis, statistics and the creation of study design. Fellows receive formal training in the use of tools such as the REDCap (Research Electronic Data Capture) survey and database application, the Duke electronic IRB system, and the DEDUCE (Duke Enterprise Data Unified Content Explorer) database query tool, which allows users to generate research questions and electronically search through millions of Duke patient records to obtain data. By the end of the fellowship year, fellows are expected to have presented their work at national meetings as well as the Duke Academic Evening and to have submitted at least one paper for publication in a scientific journal.

Duke University Medical Center is a world-renowned academic medical center. Owing to being based at a tertiary referral and level 1 trauma center, the RAAPM fellowship benefits from exposure to a highly diverse case-mix. The Department of Anesthesiology provides care for over 30,000 surgical cases per year, and performs approximately 10,000 single injection and continuous peripheral nerve blocks annually. Duke University Hospital has a well-established Inpatient Pain Service (IPS) with an interdisciplinary team approach. The Duke IPS performs an average of 500 new inpatient consults and 11,000 patient visits per year. Duke IPS also manages approximately 2,000 epidural catheters per year in addition to peripheral nerve catheter management.
Involvement in a fellowship research project is REQUIRED and assures skill development in:
- The ability to formulate clinically relevant hypotheses in regional anesthesiology and acute pain medicine
- Research design to create achievable studies that will answer questions according to scientific methods
- Execution of research project
- Introduction to statistical analysis techniques
- Interpretation of results and preparation of a manuscript
- Presentation of research at national or international meetings, which forms the basis of a peer-reviewed manuscript submission for publication
- Introduction to research funding and grants
- Ability to critically evaluate the research of other investigators

A true consultant subspecialty anesthesiologist is not only a subject matter expert and a scholar, but an educator. Duke RAAPM fellows receive training in how to effectively teach trainees and give feedback, as well as training on simulation in education. The role of the fellow in the block area naturally changes over the course of the year. Fellows begin as learners, and as they gain mastery of the technical and cognitive skills, shift in their role to being that of a teacher by the completion of fellowship, guiding resident trainees in block procedures. This is done under the supervision of a faculty member who aids in the fine-tuning of the fellows’ teaching style.
Duke RAAPM fellows are also involved in teaching local preceptorships as well as at hands-on ultrasound guided nerve block workshops around the country. Recent workshop locations have included New York City, Orlando, Washington D.C., Las Vegas, and Charleston, SC.
Regional Anesthesiology & Acute Pain Medicine fellows are taught and mentored by faculty from the Divisions of Ambulatory Anesthesiology and Orthopaedics, Plastics, and Regional Anesthesiology. Meet our faculty and find out what our Regional Anesthesiology & Acute Pain Medicine fellowship alumni have been up to!
Check out what our faculty and fellows are doing by following @Duke_Anesthesia on X and Instagram!
And don’t forget to follow division chief @jeffgadsden and his educational #Blocktober videos on YouTube.
After graduation, Duke fellowship graduates enter either private or academic practice, which varies slightly with each graduating class. To get a first-hand account of our fellowship program, we encourage you to ask our current fellows or alumni about their experiences.
2024-2025
Stephen Davies, MD
Emily Barney Hall, MD
Matt Harrell, MD, MS
Alex Loji, MD
Kevin Su, MD, PhD
2023-2024
Talitha Budi, MD
Benjamin Fiorillo, MD
Akshay Jagadeesh, MD
Dylan Matthews, MD
Ariana Prinzbach, MD
2022-2023
Christina Chen, MD
Emily Chen, MD
Ivy Co, DO
James Maher, MD
Bryan Ray, MD
2021-2022
Sophia Dunworth, MD
Gisselle Maquoit, MD
Jason Stearns, MD
Rose Tang, MD
Bella Vishnevsky, MD
2020-2021
C. Russ Horres, MD
Stephan Frangakis, MD, PhD
Brian Nevitt, MD
Andrew Wong, MD
2019-2020
Anne Castro, MD
An Chen, MD
Ken Mullen, MD
Peter Shin, MD
2018-2019
David Creighton, MD
Elizabeth Gauthier, DO
Christian Horazeck, MD
Milly Rambhia, MD
2017-2018
Kasra Razmjou, MD
Christopher Wahal, MD
Brendan Keen, MD
Lisa Kumar, MD
2016-2017
James Kim, MD
Amanda Kumar, MD
Neda Sadeghi, MD
2015-2016
Irfan Samee, MD
Siddharth Sata, DO
Evan Sutton, MD
2014-2015
William Bullock, MD
Ryan Mountjoy, MD
Jordan Taylor, MD
2013-2014
Earl Wilson, MD
Thomas Maliakal, MD
David Tunnel, DO
2012-2013
Brian Ohlendorf, MD
Stephanie Chen, MD
2011-2012
Hanni Monroe, MD
Karthikeyan Srinivasan, MD
Kavita Kantak, MD
2010-2011
Jay Kher, MD
Juliann Hobbs, MD
Michael Shaughnessy, MD
2009-2010
Patrick Armstrong, MD
Jennifer Sposito, MD
Sean Dobson, MD
2008-2009
Erin Rose, MD
Mitchell Fingerman, MD
Joshua Dooley, MD
2007-2008
Kristie Osteen, MD
2006-2007
David Auyong, MD
Jeffrey Gonzales, MD
James Benonis, MD
2005-2006
Reginald Julien, MD
Fernando Altermatt, MD
2004-2005
Robert Schlosser, MD
2003-2004
Scott Croll, MD
Holly Evans, MD
2002-2003
Trenton Pierce, MD
Nadeem Ahmed, MD
2001-2002
Chester “Trip” Buckenmaier, III, MD
Yair Rubin, MD
Adil Kamar, MD
1999-2000
Karen Nielsen, MD
Stuart Grant, MD
1998-1999
Jennifer Charlton, MD

Find out why Durham, North Carolina is a great place to work and play.