Q: Why does the Duke Anesthesiology Residency Program believe it’s important to offer trainees “near-peer teaching?”
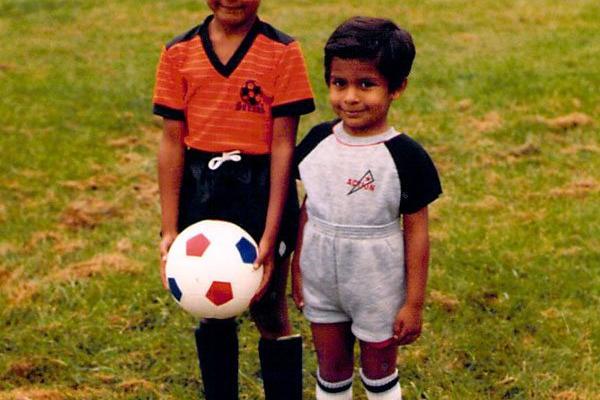
A: During childhood, I would not admit it, but now I am proud to say I learned a lot from my older brother. He is two years older than me and taught me skills such as catching a football, packing my lunch, dealing with bullies and more. Why is it easier to learn certain skills from a sibling compared to parents? Educational theorists give many reasons, probably the most important being the knowledge gap between an expert and a beginner compared to the gap between a beginner and someone with intermediate skill. There is also an intimidation factor in a novice who is asking for assistance from an expert (Melvin 2014).
Inherently, anesthesiology resident education does not provide many opportunities for near-peer teaching, or teaching of CA1 residents by CA2 and CA3 residents. In fact, anesthesiology is one of a few medical specialties that actually pairs novice residents with experts in an operating room environment. It is common for a CA1 resident with less than three months experience to be learning from an anesthesiologist with more than 10 years of experience, daily!
As educators, we need to provide ample opportunities for near-peer teaching. Some examples in our Duke Anesthesiology Residency Program and others around the country include:
- Teaching scholars program: CA3 residents interested in education are elected into leadership positions to help with teaching activities for medical students and junior residents using simulation, lecture-based and intraoperative environments.
- Advanced clinical rotation: CA3 residents are assigned to coach CA1 and CA2 residents through advanced anesthetic cases.
- Social activities: Promote team building between classes (scavenger hunt, retreats, informal and formal dinner gatherings).
- Team night float system: Same CA3 and CA1 work together for an entire week on night call.
- Simulation activities teaching crisis management while senior residents are working with junior residents on difficult anesthetic cases.
There is a role to train residents and medical students to be effective teachers. Near-peer teaching does not end with residency, it is a lifelong necessity - and not limited to work only. I still learn from my brother.
Melvin, L et al. What makes a great resident teacher? A multi-center survey of medical students attending internal medicine conference. JGME. 2014. Available at: http://www.jgme.org/doi/pdf/10.4300/JGME-D-13-00426

