
The National Institutes of Health’s National Institute on Aging has awarded more than $4.5 million in grants to Duke Anesthesiology’s Niccolò Terrando, PhD, and teams to study the impact of surgery on the vulnerable brain.
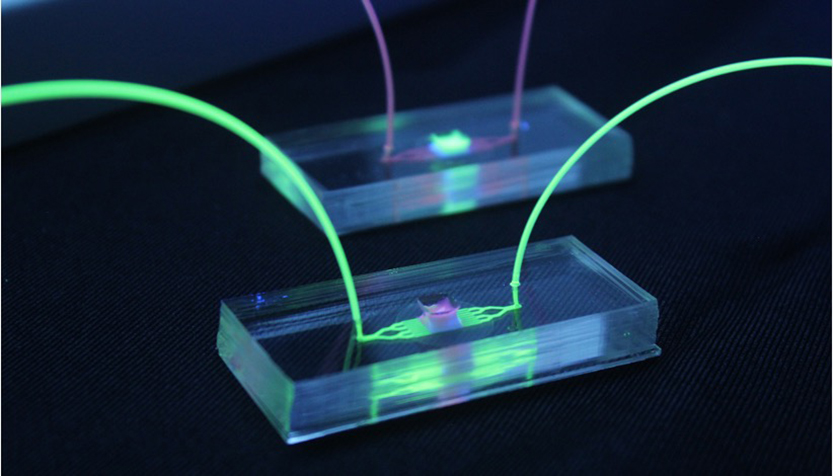
The first RF1 project, titled “Immunovascular Interactions in Postoperative Delirium Superimposed on Dementia (DSD),” builds on a long-term collaboration with Dr. Harris Gelbard of the University of Rochester that continues to characterize changes in the blood-brain barrier following orthopaedic surgery during ongoing neurodegenerative pathology. The current project leverages a specific technology comprised of microphysiologic system with nanoporous silicon membranes (μSiM) populated with human induced pluripotent stem cells (iPSCs), a platform pioneered by co-investigator Dr. James McGrath, also of the University of Rochester.
“These devices are providing new opportunities to model complex processes of postoperative delirium with the goal of better defining the neurovascular changes affecting the vulnerable brain after anesthesia and surgery,” says Terrando. “This work will expand our understanding of how surgery affects the blood-brain interface and will provide new molecular mechanisms of relevance to delirium during aging and neurodegeneration.”
Such knowledge is significant because it will implement new technologies to investigate immune-vascular interactions and inform the advancement of safe therapies to limit postoperative neurocognitive complications in vulnerable patients.
“We view this award as truly transformative: the field of DSD research has largely relied on murine transgenic models that do not necessarily translate into platforms that lead to translational advances in new therapies targeting neuroimmune interventions at the blood-brain barrier,” says Gelbard. “By using Dr. McGrath’s platform with human iPSCs, we hope to inform and advance Dr. Terrando’s in vivo models in ways that lead to clinically relevant advances in our understanding of DSD.”
The second RF1 project, titled “Understanding the Role of Senescence on Postoperative Neuroinflammation,” is in collaboration with Dr. Shyni Varghese of Duke Orthopaedic Surgery. It is long known that advanced age is a key risk factor for delirium and perioperative neurocognitive disorders, however, the mechanisms whereby aging contributes to excessing and non-resolving neuroinflammation in some subjects after surgery remains unknown. This project will evaluate the role of senescence, a process implicated in cellular aging and inflammation, as a key driver of neuroinflammation in postoperative delirium. This project will test if and how senolytics, drugs currently tested in humans for other disorders including Alzheimer’s disease, protect from surgery-induced neuroinflammation and delirium-like behavior in aged and transgenic models. Investigators will also focus on the reciprocal interactions between the blood-borne factors and the blood-brain barrier using a microphysiological system as recently published by the Varghese and Terrando laboratories.
“Our department is incredibly proud of this cutting-edge work that stands to revolutionize the way we study the neuroinflammatory changes occurring in the perioperative period,” says Miriam Treggiari, MD, Duke Anesthesiology vice chair for research. “No team is better positioned to perform this highly translatable work and to bring us closer to discoveries that we can evaluate in human subjects in the future.”
The intersection of advanced age and neurodegeneration, two key risk factors for postoperative cognitive complications, represent a growing epidemic for our society with important repercussions on patient outcomes and significant challenges to our health care system. The Neuroinflammation and Cognitive Outcomes Laboratory, led by Terrando, faculty of Duke Anesthesiology’s Center for Translational Pain Medicine, is dedicated to understanding how surgery impacts cognitive outcomes in vulnerable subjects. "We are grateful for the support from the National Institute on Aging to expand our research program and collaborative footprint to develop new tools to clarify the complex multifactorial etiology of delirium," says Terrando.