Lab Description
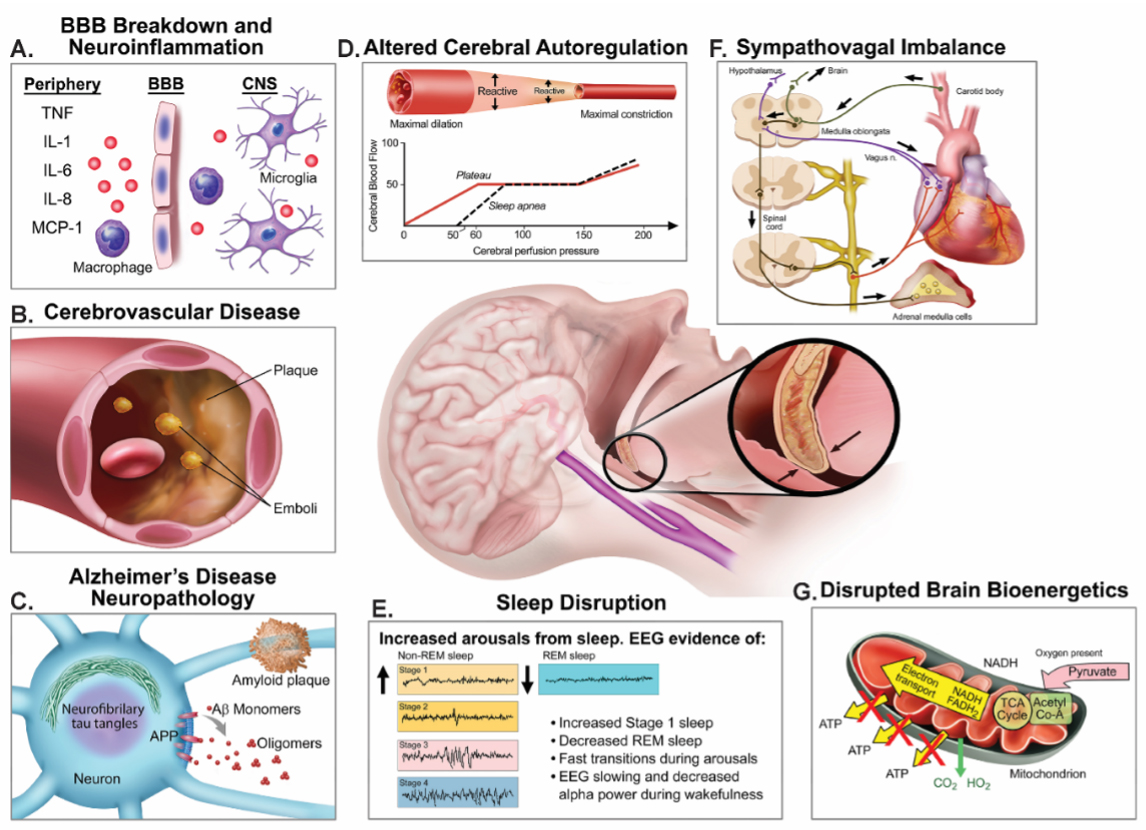
The Critical Illness and Perioperative Brain Health Research (CIPHER) Laboratory is dedicated to improving brain health in older surgical and intensive care unit (ICU) patients. We are particularly interested in delirium (in both postoperative and ICU patients) and its sequalae such as long-term cognitive impairment. We conduct human clinical-translational studies to better understand the neurobiological underpinnings of delirium, post-ICU syndrome, long-term cognitive impairment, and Alzheimer’s disease and related dementias. These studies employ multimodal techniques, including EEG, pupillometry, neuroimaging, and plasma and cerebrospinal fluid biomarkers (proteomics, ELISA based assays).
Lab Opportunities
The lab is always looking for interested graduate and medical students to join our team. We are also seeking a visiting research scholar with experience in EEG sleep scoring. Interested candidates should email their CV and cover letter describing their research interests.
Research Interests
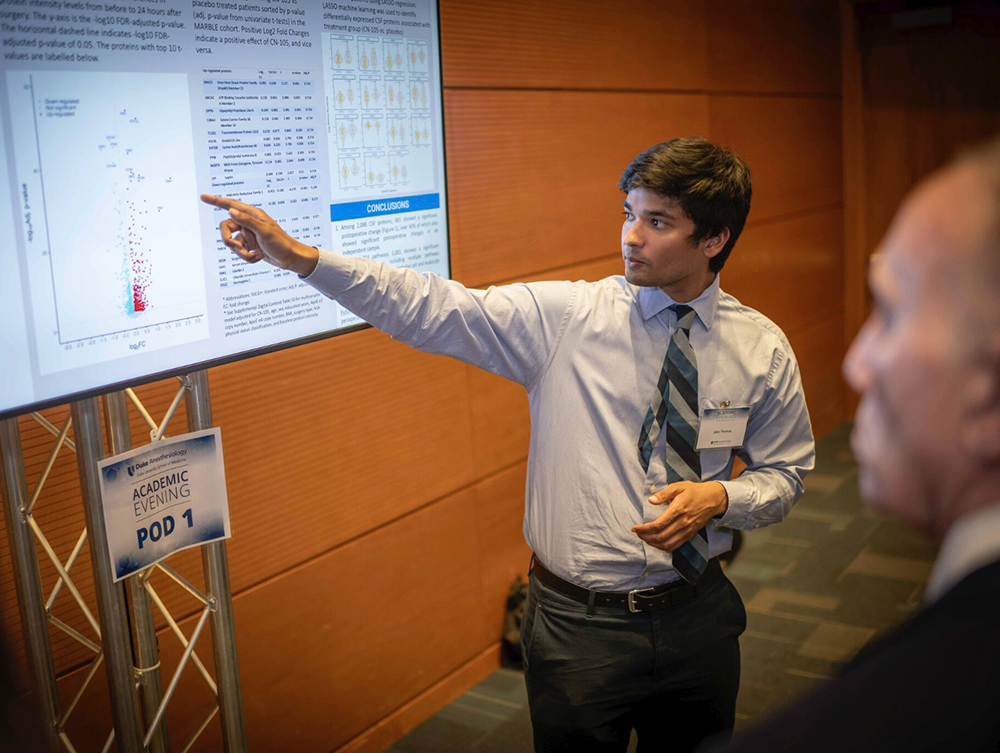
The Role of Neuroinflammation and Blood-brain Barrier Dysfunction in Perioperative and Intensive Care Unit (ICU)-Acquired Neurocognitive Disorders
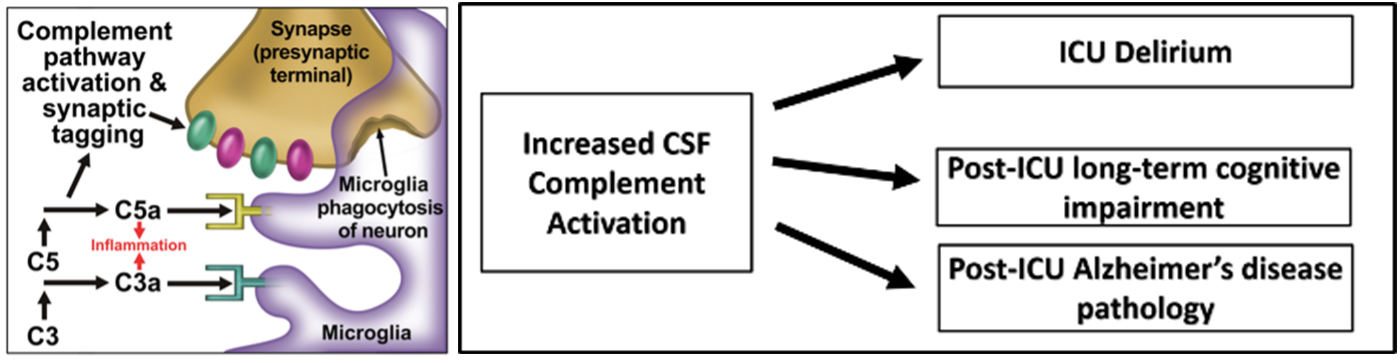
Using our perioperative CSF biorepository, we are currently investigating the role of complement activation and other neuroinflammatory pathways in postoperative delirium and neurocognitive disorders.
We are also conducting an NIA-funded study CASCADE-ICU to investigate the role of complement pathway activation in ICU-delirium and post-ICU long-term cognitive impairment. With the help of the Duke/UNC ADRC, we are also investigating synaptic injury and Alzheimer’s disease biomarker changes in older ICU patients.
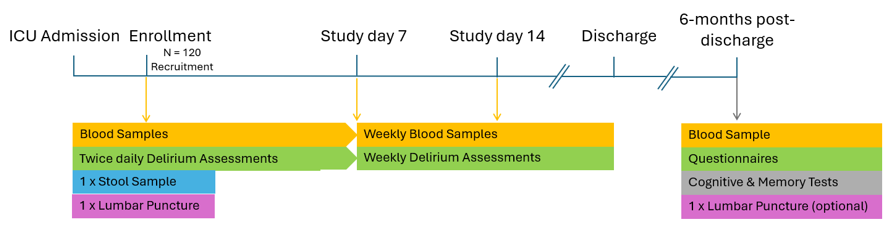
In CASCADE-ICU, we are investigating the neurobiological underpinnings of ICU delirium and post-ICU long-term cognitive impairment. We hypothesize that cerebrospinal fluid (CSF) complement pathway activation during critical illness is associated with ICU delirium and post-ICU long term cognitive impairment. To answer this question, we are enrolling 120 age>= 65 ICU patients that will undergo CSF and blood sampling, delirium assessments and follow-up cognitive testing at 6-months, 1 year, and 3 years following hospital discharge. CSF complement pathway activation will be measured with mass spec proteomics and immunoassays. CSF and blood samples obtained here are also stored in a biorepository to enable future investigations of other mechanisms of ICU delirium.
Funding: NIA K23AG084898, Duke/UNC Alzheimer’s Disease Research Center Development Project Award, National Alzheimer’s Coordinating Center Junior Investigator Award (Completed)
References:
- Role of Blood-Brain Barrier Dysfunction in Delirium Following Non-cardiac Surgery in Older Adults.
- Cognitive and Cerebrospinal Fluid Alzheimer's Disease-Related Biomarker Trajectories in Older Surgical Patients and Matched Nonsurgical Controls.
- Immunomodulatory Lipid Mediator Profiling of Cerebrospinal Fluid Following Surgery in Older Adults.
- Cerebrospinal Fluid Proteome Changes in Older Non-Cardiac Surgical Patients with Postoperative Cognitive Dysfunction.
The Role of Sleep Disruptions in Postoperative and ICU Delirium
Given emerging evidence showing that adequate sleep is important to brain health, we are investigating whether sleep disruptions are associated with perioperative and ICU-acquired neurocognitive disorders. In our prior SANDMAN (Sleep Apnea, Neuroinflammation, and Cognitive Dysfunction Manifesting After Non-cardiac surgery) study we investigated the role of sleep apnea in perioperative neurocognitive disorders (10.1213/ANE.0000000000007269). Surprisingly, we found that undiagnosed sleep apnea was not a risk factor for delirium or postoperative neurocognitive disorder. Thus, our attention has turned to sleep disruptions as a risk factor, and our current studies are using in-hospital EEG to quantify sleep patterns in patients at risk for delirium. We are also investigating sleep-related changes in sustained attention following surgery.
Funding: NIA R03AG067976 (Completed), Foundation for Anesthesia and Education Research Fellowship Grant (Completed)
References:
Postoperative Pharmacologic Sleep Modulation to Prevent Postoperative Delirium
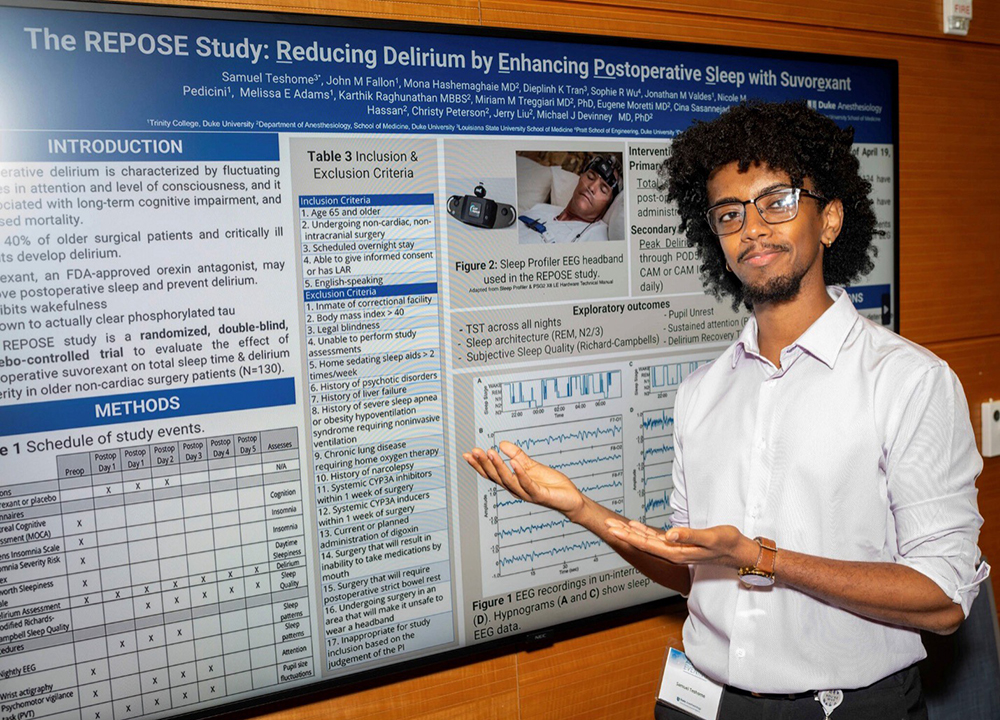
We are carrying out a study to determine whether postoperative sleep enhancement with the orexin antagonist suvorexant increases postoperative sleep and reduces delirium severity. The REPOSE study (reducing delirium by enhancing postoperative sleep with suvorexant; NCT05733286) is a single-center, randomized, double-blind RCT that aims to evaluate the efficacy of suvorexant in increasing total sleep time and decreasing delirium in older patients undergoing non-cardiac surgery. In REPOSE, 130 older non-cardiac non-neurologic surgery patients will be randomized to receive 20 mg suvorexant vs placebo for the first three nights after surgery and undergo delirium assessments and sleep measurement with an EEG headband. Within REPOSE, we are also conducting pilot studies on the relationship of postoperative changes in sustained attention and pupillary unrest in ambient light with postoperative delirium. REPOSE is funded by an investigator-initiated study from Merck.
Funding: Investigator-Initiated grant from Merck Investigator Studies Program
Anesthesia as a Stress Test to Reveal Delirium and Dementia Risk in Older Surgical Patients
It has been well known that lower anesthetic dose is needed to provide anesthesia for older adults, but few studies have determined whether anesthetic dose requirements and EEG responses to anesthesia indicate pre-existing dementia pathology and risk for postoperative delirium. Thus, with my mentor Dr. Miles Berger, I am co-leading a study to investigate whether anesthetic-dose adjusted EEG responses are associated with increased Alzheimer’s disease CSF biomarkers, functional MRI connectivity changes, neurovascular dementia risk and increased risk for postoperative delirium. To accomplish this, 250 older non-cardiac surgery patients that require general anesthesia will undergo preoperative lumbar puncture, fMRI, and postoperative delirium assessments in the NIA R01-funded ALADDIN study: Low Neurophysiologic Resistance to Anesthetics as a Marker of Preclinical/Prodromal Alzheimer's Disease and Neurovascular Pathology, Delirium risk and Inattention.
Funding: NIA R01AG073598 (co-PI with Stanford Collaborator Dr. Miles Berger)
Lab Members
Lab Manager/Research Program Project Leader
Scholars/Postdocs
Clinical Research Coordinators (CRC)
Clinical Research Specialists, Sr (CRS)
Medical/Graduate Students

Shivam Chand, BS
Bioethics and Science Policy Graduate Student

Jacqueline Emerson, BS
Medical Student

Kristen Monten, BS
Medical Student

Sam Teshome, BS
Medical Student
Undergraduate Students

Sabina Ferrari
Duke Class of 2027

Cole Kannam
Duke Class of 2027

Jerry Liu
Duke Class of 2027

Will McIntosh
Duke Class of 2026

Nicole Pedicini
Duke Class of 2026

Vinith Upadhya
Duke Class of 2026
Local Collaborators
Gow Arepally, MD
Professor of Medicine
Duke, Department of Medicine
Jeffrey Browndyke, PhD
Associate Professor of Psychiatry and Behavioral Sciences
Duke, Department of Psychiatry & Behavioral Sciences
Mary Cooter, MS
Biostatistician
Duke, Department of Anesthesiology
Duke Molecular Physiology Institute
James Bain, PhD
Janet Huebner, MS
Mike Muehlbauer, PhD
Duke Proteomics Core Facility
Matthew Foster
Michael Lutz, PhD
Professor in Neurology & Pathology
Duke, Department of Neurology
Joseph P. Mathew, MD, MBA, MHSc
Jerry Reves Professor & Chair
Duke, Department of Anesthesiology
Eugene Moretti, MD, MHSc, FASA
Professor of Anesthesiology
Duke, Department of Anesthesiology
Cina Sasannejad, MD
Assistant Professor of Neurology
Duke, Department of Neurology
Mara Serbanescu, MD
Assistant Professor in Anesthesiology
Duke, Department of Anesthesiology
Dr. Niccolo Terrando
Associate Professor
Duke, Department of Anesthesiology
Miriam Treggiari, MD, PhD, MPH
Paul G. Barash Professor of Anesthesiology
Duke, Department of Anesthesiology
Dr. Heather Whitson
Duke Center for the Study of Aging & Human Development
Duke, Department of Medicine, Geriatrics Division
Dr. Marty Woldorff
Duke Center for Cognitive Neuroscience & Department of Psychology & Neuroscience
Hoatian Zhu, PhD
Postdoctoral Associate
Stanford University Collaborators

Miles Berger, MD, PhD
Professor of Anesthesiology, Perioperative and Pain Medicine

Ghazal Masarweh
Clinical Research Coordinator Associate

Melody Reese, PhD
Postdoctoral Fellow
External Collaborators
E. Wes Ely, MD, MPH
Professor of Medicine
Grant W. Liddle Chair in Medicine
Co-Director Cent for Critical Illness, Brain Dysfunction, and Survivorship
Vanderbilt University Medical Center
Henrik Zetterberg, MD, PhD
University of Gothenberg
Sweden
In the News
Dr. Devinney Awarded Grant to Further Study Underlying Mechanisms of Delirium
Duke Delirium Research Earns ISTAART Accolade
Dr. Devinney Earns Prestigious Accolade for Research on Aging
Dr. Devinney Earns New Investigator Award for Alzheimer's Research
Dr. Devinney Awarded Grant for Aging and Delirium Research
External News
2025
Congratulations to CIPHER Lab member, Dr. Tyler Reekes, on his online publication on MEDRXIV titled, “Predilection for Perplexion: Preoperative microstructural damage is linked to postoperative delirium,” which provides a novel neuroanatomic explanation (i.e. microstructural dysfunction within the posterior cingulate cortex) for the long-observed association between preoperative cognitive impairment and postoperative delirium risk among older surgical patients.
Publications
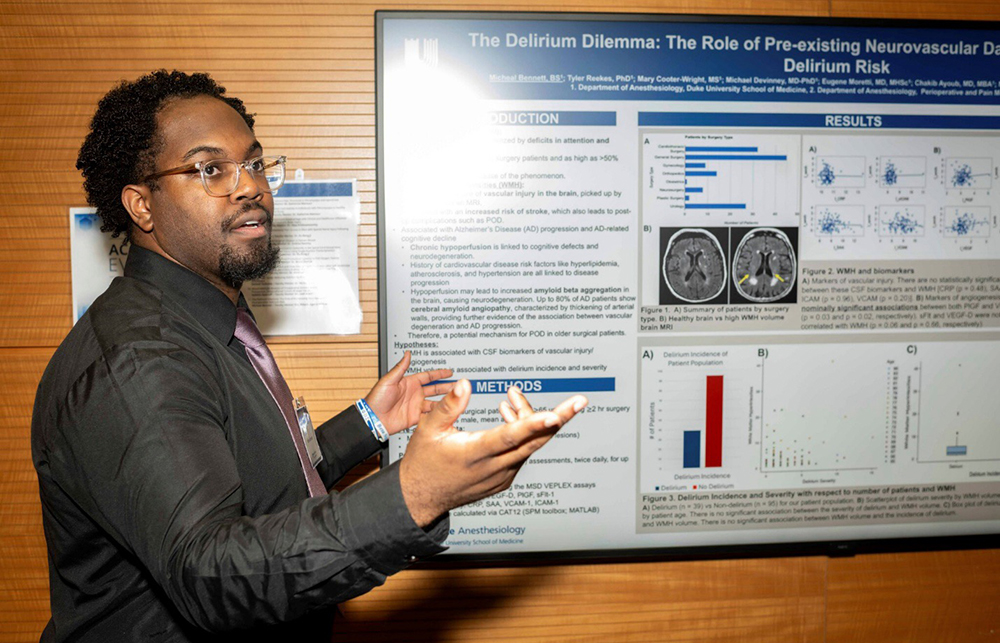
Photos











Study Contact
ALADDIN Study
Piper Boykin
Clinical Research Coordinator
919-660-9396
ALADDINstudy@duke.edu
CASPER Study
Bethany Hsia, PhD
Research Program Leader
919-660-9364
bethany.brown@duke.edu
CASCADE-ICU Study
Noah Timko
Clinical Research Coordinator
919-660-0376
CASCADE-ICU@duke.edu
REPOSE Study
Christy Peterson
Clinical Research Coordinator
919-681-3579
REPOSE@duke.edu