It is impossible to recount the history of Duke Anesthesiology without mentioning The Center for Hyperbaric Medicine and Environmental Physiology (CHMEP). The histories of these two entities are undeniably linked. The CHMEP played a significant role in shaping and defining Duke Anesthesiology as a department, and consequently, in defining the numerous divisions that have been established over time. Perhaps even more importantly, the exciting work being done at the CHMEP today will play a significant role in defining both our future as a department, as well as the future potential of human exploration.
A multidisciplinary facility, the CHMEP conducts research and provides clinical services to patients in need of pressure and oxygen as a form of treatment. The CHMEP was established as an academic center in 1986. Prior to 1986, hyperbaric and physiological research was limited to the F.G. Hall Laboratory, which is still a part of the CHMEP today. The F.G. Hall Laboratory was created in 1963 with funds provided by the National Institutes of Health (NIH). It began as a chamber complex with the ability to simulate pressure ranging from depths of 1,000 feet of seawater to 100,000 feet of altitude.
When Merel H. Harmel, MD, arrived at Duke in 1971 to chair the newly created Department of Anesthesiology, he was disappointed to learn that the department had no laboratory and, consequently, no research activity. At that time, the F.G. Hall Laboratory was affiliated with the departments of surgery and medicine, and was under the direction of Herbert Saltzman, MD. Soon after Drs. Saltzman and Harmel were introduced, they realized that the Department of Anesthesiology would be an ideal sponsor for the laboratory and would provide the fledgling department a turn-key facility with a well-established research reputation. The Department of Anesthesiology has sponsored the F. G. Hall Laboratory since 1972.
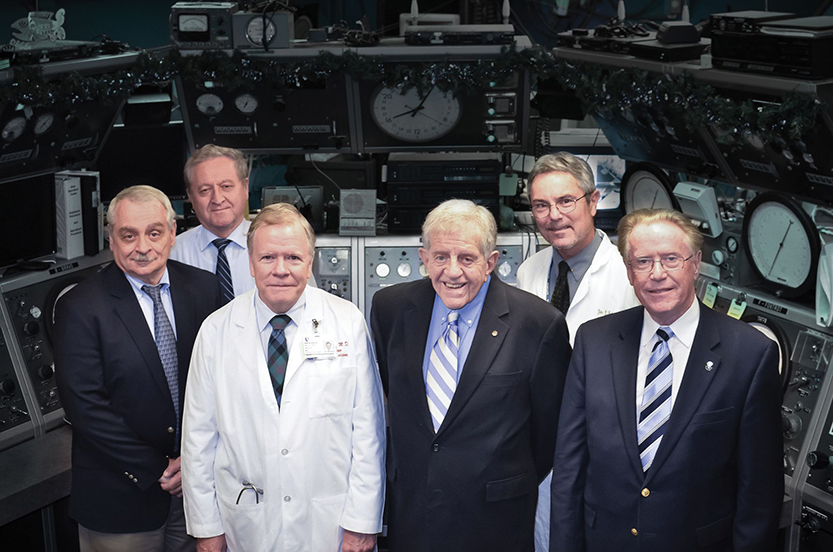
Together, Drs. Saltzman and Harmel recruited a bright young man from England, Peter Bennett, PhD, DSc, to serve as Duke Anesthesiology’s first director of research and co-director of the hyperbaric program. One of Dr. Bennett’s first goals was to strengthen the lab’s financial support. The best way to do this was to develop a strong clinical component to attract support from commercial and government agencies. With that goal in mind, Dr. Bennett recruited additional world-class physicians including Lennart Fagraeus, MD, Enrico Camporesi, MD, John Miller, MD, Richard E. Moon, MD, CM, MSc, FRCPC, who now serves as medical director, and Claude A. Piantadosi, MD, current director of the CHMEP. As a result of this collaborative effort, the laboratory’s funding increased tenfold. In 1980, Dr. Bennett founded the Divers Alert Network (DAN), an emergency hotline for recreational divers, now a $16 million non-profit organization.
This increased financial support helped bolster the lab’s research initiatives, which had already gained international acclaim. The F.G. Hall Laboratory’s earliest experiments focused on mechanisms of anesthesia and deep diving physiology. At that time, ocean exploration was severely limited because of nitrogen narcosis and High Pressure Nervous Syndrome (HPNS). Both effects are caused by extreme pressure on the human body.
The early work of Johannes Kylstra, MD, had practical implications to both deep-sea exploration and clinical medicine. Dr. Kylstra conducted a number of experiments related to respiration of oxygen-rich liquids. He was the first to prove that land animals could breathe liquids, and he later conducted the first human liquid breathing trial. Throughout the 1970s, the faculty continued to conduct liquid breathing experiments. Although liquid breathing in humans has not yet been put into practice, these experiments were instrumental in developing the lung lavage technique and in elucidating the HPNS mechanism.
The lung lavage technique involves washing out one lung with a mild salt solution while ventilating the second lung with pure oxygen. The CHMEP is among the few facilities in the world equipped with the necessary pressure chambers and personnel required to safely complete this procedure, which is commonly used to relieve the symptoms of pulmonary alveolar proteinosis.
Furthermore, with this discovery, Dr. Bennett was able to prove that HPNS is not caused by the gases breathed at intense pressure, but by the pressure itself. This led to the development of a mixture of nitrogen, helium and oxygen known as TRIMIX, which Dr. Bennett believed could effectively eliminate the symptoms of HPNS. In 1968, Dr. Saltzman had achieved simulated dives to the equivalent pressure of 1,000 feet in collaboration with the U.S. Navy. Dr. Bennett was anxious to see if he could break this record and obtain simulated depths of 2,000 feet.
In 1976, the Navy sponsored the installation of two new chambers in the F.G. Hall Laboratory with the capability to achieve a simulated depth of 3,600 feet using a wet chamber so that Duke faculty could explore the limitations of the human body at even greater depths. Thus began a series of four highly acclaimed experiments known as the Atlantis Dives in which human volunteers were locked inside seven-foot-wide steel chambers for weeks at a time and subjected to extreme pressure. The success of these experiments depended on the proper composition of TRIMIX for the volunteers to breathe. During the Atlantis III experiment in 1981, three volunteer divers successfully reached depths of 2,250 feet, breaking the existing world record.
In addition to pushing the limits of underwater exploration, the CHMEP has a history of collaboration with the National Aeronautics and Space Administration (NASA). In fact, the physiologist after whom the laboratory was named—Frank Gregory Hall—contributed to the development of the pressure suits that NASA astronauts use today. The center was instrumental in developing decompression tables enabling construction of the International Space Station. Over the years, the CHMEP researchers have honed the procedures for proper suit decompression so that astronauts can safely participate in extravehicular activity. In recognition of these efforts, the Duke flag has flown aboard the International Space Station.
Currently, research at the CHMEP focuses on cardiopulmonary physiology, free radical biology, and oxygen biochemistry. “Although we have used hyperbaric oxygen as a treatment method for years,” explains Dr. Piantadosi, “we are still trying to understand how and why this works at the biochemical and molecular level.” A new area of research suggests that oxygen derivatives act as signals for the body, stimulating its natural protective response to cellular injury. If this is correct, the use of hyperbaric oxygen could help improve the health and homeostasis of many body systems in a wide range of diseases. The CHMEP’s future goals will focus on obtaining a better understanding of these potential applications.
When Dr. Harmel acquired the F.G. Hall Laboratory, he gained much more than a convenient location to develop the department’s research component. This relationship instilled a strong spirit of inquiry within the young anesthesia department, which is still evident today in each subspecialty that has formed within the department. As long as this curiosity is maintained, the potential for future discovery is limitless.